hen something bad happens whether it is out in the world or at work, it can be hard to know the right thing to say. News channels have always shared a stream of violence, yet over the last few years it can feel closer to home. And when our communities experience trauma, health care workers feel those effects, too. This is in addition to the already common experience of traumatic events in healthcare. Across clinical spaces, healthcare workers see health and healing, but we also see death and dying. We see mistakes happen, we make difficult decisions and the outcomes aren’t always as expected. People are people. Sometimes we get angry and say things we shouldn’t. Much of our work is out of our control. This occupational trauma (trauma that happens at work) can be hard to manage. In the long run, they can contribute negatively to our mental health. There are, though, ways to help ourselves and our teams manage these stresses and support each other in the process.
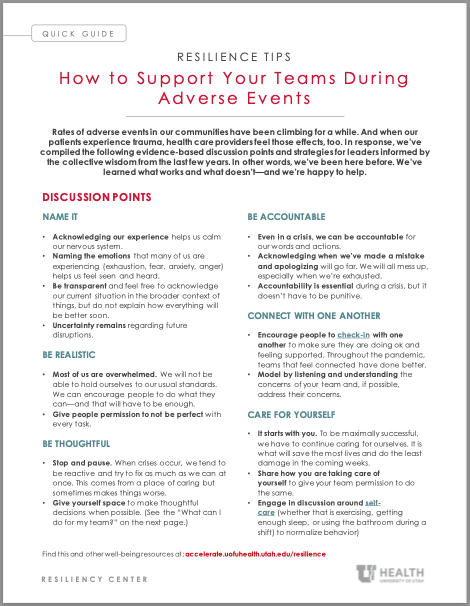
The following is a compilation of evidence-based discussion points and strategies for leaders to empower teams to better cope with the avalanche of adverse events that are an inevitable part of working in health care. informed by the collective wisdom of the last two years. In other words, we’ve been here before. We’ve learned what works and what doesn’t—and we’re happy to help.
In short, we can help. There’s hope and relief in the collective wisdom of our peers and the solidarity of our teams.
Talking points for after an adverse event
Name It |
|
Be Realistic |
|
| Be Thoughtful |
|
| Be Accountable |
|
| Connect with One Another |
|
| Care for Yourself |
|
What can I do for my team?
There are three key ways to help a team. The following seven questions can help prioritize and guide action. The first five are particularly useful in times of crisis.
Connect as humans and build trust
| Questions to ask | Why it helps |
|---|---|
| 1. Does your team feel a strong sense of connection? | Connection is a key ingredient for groups that are doing well. |
| 2. Does your team feel supported (by you, each other, the department/ system)? Do they feel seen, valued, and heard? | Communication, recognition and support can occur in many ways. |
Recognize and talk about occupational trauma
| Questions to ask | Why it helps |
|---|---|
| 3. Do they have an opportunity to debrief about their experiences? | Reach out for help from the Resiliency Center if needed. |
Empower the team to make things better
| Questions to ask | Why it helps |
|---|---|
| 4. Does the department/division/clinic have the resources needed to succeed? | Be an advocate for resources even when resources are scarce. Allow yourself to be creative. |
| 5. Are you able to identify the biggest obstacles for your group? | Pick one issue to work on (not fix) to address an upstream driver of burnout/ dissatisfaction. |
|
6. Are you discussing professional development in a coaching framework? |
Support a connection to purpose that also has a direction. |
| 7. Are your people empowered to change what is in their local area of control? | Provide a framework to allow autonomy for everyone to pitch in. |
What if someone on my team is really struggling?
There are a wealth of resources available for those in crisis or in urgent need of help. As always, stay connected by visiting the Resiliency Center updates on Pulse.
Crisis Resources
Huntsman Mental Health Institute (HMHI)
-
Crisis Line: 801-587-3000, available 24/7, 365 days/yr
-
Warm Line: 801-587-1055, available 8am-11pm, 365 days/yr
-
SafeUT Frontline: 801-372-3335 or https://safeut.org/frontline
Employee Assistance Program
-
Phone: 801-262-9619, this is also a crisis line 24/7, 365 days/yr
-
Daily Crisis Appointments Available, includes 1-hour/day at the Resiliency Center
-
CALL AHEAD to schedule an appointment, do not walk-in
National Crisis Call & Text Lines
-
Call 800-273-8255
-
Text HOME to 741741
Urgent Resources
-
Frontline Urgent Referral (email on Pulse website) or contact your PCP
-
Resiliency Center: 801-213-3403 or resiliencycenter@hsc.utah.edu
-
GME Wellness: 801-213-8753 or GMEwellness@hsc.utah.edu
-
University Counseling Center: 801-581-6826
Megan Call
Amy Locke
How do I share employee engagement feedback with my team? Chief Wellness Officer Amy Locke, Resiliency Center director Megan Call, Utah Health Academics HR leader Sarah Wilson, and Organizational Development Director Chris Fairbank explain when and how to talk with your team.
Dentist Gary Lowder has spent the past 36 years working with patients who suffer from jaw disorders that result in chronic pain. As faculty in the School of Dentistry, he’s passing along the power of vulnerability as a patient trust-building exercise with his trainees.
Chief Wellness Officer Amy Locke shares practical strategies for leaders to address the real tension we’re feeling between the desire to take a break and the increasing workload.