e’re finally coming to a point in the pandemic where people are asking, “Okay, things really need to get better. How do we dig ourselves out of this burnout cycle?”
One of the best strategies I’ve used is called Listen-Sort-Empower. Developed in 2016 by then Mayo Chief Quality Officer Stephen Swensen, Listen-Sort-Empower is a simple, three-part framework that helps teams “listen” to each other and identify opportunities for improvement, “sort” to decide what to focus on, and “empower” to lead the change, rather than rely on leadership or outside intervention.
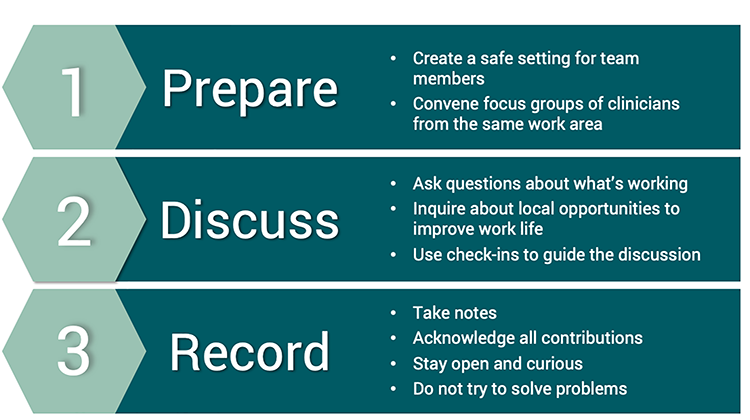
LISTEN – Your team can identify local opportunities for improvement
Question Guide for Teams
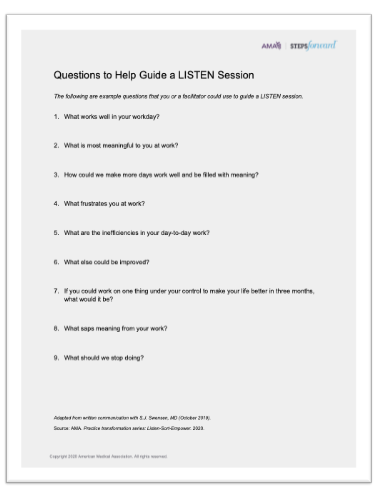
Swensen provides a list of questions to lead and facilitate a discussion with your team. Using “appreciative inquiry” to build on what already works well.
Welcome all ideas. Listening involves open and honest discussion of what’s working and what isn’t. It has to be a no-blame, no-shame, any-idea-goes exercise. Shutting someone down, even once, can prevent important information from surfacing. If people don’t feel comfortable speaking openly on your team, I strongly encourage you to think about a facilitator. The Resiliency Center offers this service to U of U Health teams. Other possible facilitators include Organizational Development for Hospitals and Clinics, and embedded Human Resources on the Health Academic side. If your team feels comfortable diving in, go for it.
Use appreciative inquiry to promote positive change. Approaching burnout from an appreciative inquiry or positive inquiry approach is helpful. Appreciative inquiry is a management approach that identifies what’s already working well to build upon or adapt and spread. As a side benefit, recognizing what’s going well can help revitalize practice.
Focus on local opportunities. Many, if not most, of the problems in health care are big, systemic challenges with no easy fix. For this activity, we want to keep the conversation focused on local opportunities that are within the team’s control to solve.
Resist the urge to “fix it.” Try and avoid problem-solving at this point. Stay out of the weeds and brainstorm. Improvement starts after we have a clearly identified what to focus on. It’s okay to have a big messy list of “to-do’s.”
Keep the group small. The ideal group for this is somewhere in the 6 to 10 range. Larger groups can be challenging. Breaking into smaller focus groups can help. Who to include is also important. If a group of physicians get together and decide, "Hey, for this clinic, we're going to do X, Y, Z,"—but there aren't any nurses, medical assistants in the discussion—it isn’t going to end well. Make sure you have a small, representative group—everyone you will need to achieve successful change needs to be at the table
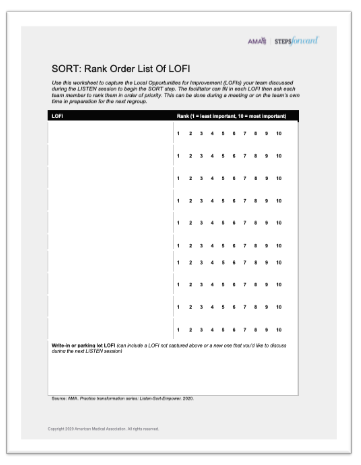
SORT – Prioritize opportunities
Once you’ve identified the list of local opportunities, it’s time to sort them by feasibility and impact. First, you want to decide if the projects you are considering have the right level of control. Swensen’s model provides three simple categories to guide the process:
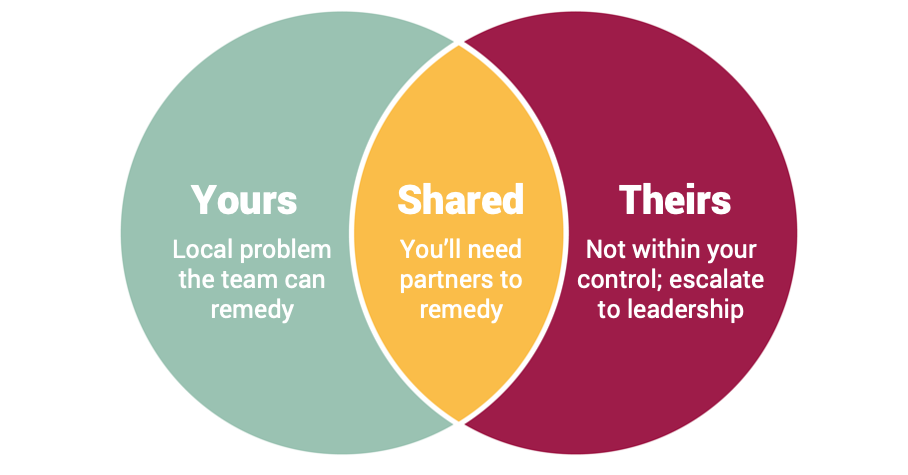
Yours – Local control to remedy
These are problems you can solve on your own. They still require adequate resources—time, talent, funding—and leadership support or sponsorship, but manageable locally.
Shared – Shared control to remedy
For opportunities that require other departments or teams, you will also need partnership. Partnership from administrative units (e.g., HR, IT, decision support), or with facilities like the hospital, inpatient units and outpatient settings all have different processes and leadership structures. Trickier, but this type of collaboration happens every day in our organization.
Theirs – No control to remedy
Large, system-wide efforts require executive sponsorship, and on the academic side, require approval from deans or chairs. These big ideas are also important to identify. Your team can pass these ideas on to those who do have control. The purpose of this exercise; however, is to focus on those things that can be addressed locally.

Once you have a list of possible targets that within the control of the group, it is time to prioritize.
High Impact, Low Feasibility = defer until resources and support secured
Maybe you find a big project idea that’s really worth it. Ask yourself, "Do we have the resources and the support available to actually act on that right now?" As we continue to see the Covid numbers decline, it might be feasible. However, we’re all pretty tired and short staffed. Is it really a good time to take on a big project? Maybe. But really have an honest conversation about what else will have to be set aside in order for it to be successful.
High Feasibility, Low Impact = defer indefinitely
If the impact is low, even if it's super easy to accomplish, it still takes time. Small wins are important, but they really need to be meaningful.
Priority #1 = High Feasibility and Impact
What you’re really looking for is the sweet spot–high impact and you have the resources and the tools to be successful.
Empower – Apply your improvement skills
Once you’ve identified an effort to focus on, you’re ready to enter the “Empower” phase. The rapid innovation approaches—standard QI and value improvement—that we use every day to improve patient care also apply to improving our professional well-being.
Trust builds authentic teams. For leaders of teams, it’s important to encourage autonomy. The Listen-Sort-Empower model is successful because it sends an important message: I hear you; I acknowledge your expertise and I trust you to be able to make it better. It encourages teams to take ownership instead of the us-versus-them mentality of, “They're making us do this thing." Working through a problem together builds camaraderie, helps people feel less hopeless, and brings meaning and purpose to the work. It shows us that we can make a difference.
Take it slow. Best practices, like piloting our interventions, slowly rolling out implementation, and spreading what works to other areas, can make change more manageable.
Learn from others. If you haven’t done an improvement project before, there are a wealth of local resources to guide you step-by-step through the improvement and problem solving process. If you want to learn what others with similar problems have done, or check out best practices for addressing burnout related to clinic issues, I suggest visiting the AMA Steps Forward modules. The AMA is geared to physicians, but any discipline can adapt the tools to meet their unique needs. Although the Listen-Sort-Empower model was created with clinical teams in mind, the process applies to any group who wants to get to work solving problems, making the University of Utah a great place to work and learn.
*Originally published February 2022
Amy Locke
How do I share employee engagement feedback with my team? Chief Wellness Officer Amy Locke, Resiliency Center director Megan Call, Utah Health Academics HR leader Sarah Wilson, and Organizational Development Director Chris Fairbank explain when and how to talk with your team.
Chief Wellness Officer Amy Locke shares practical strategies for leaders to address the real tension we’re feeling between the desire to take a break and the increasing workload.
To disagree means failing to agree. Synonyms include to contradict, challenge or debate. Synonyms do not also have to include to argue, quarrel, dispute, bicker or clash. Pediatric intensivist Jared Henricksen shares the best path forward when words become clouded with emotion.