ow—more than ever—stress and burnout are affecting our work. In the Resiliency Center, we are seeing more teams, not just individuals, showing signs of fatigue. With a little data and some introspection, you can make a difference for your team.
Here are three questions to help you find your starting point:
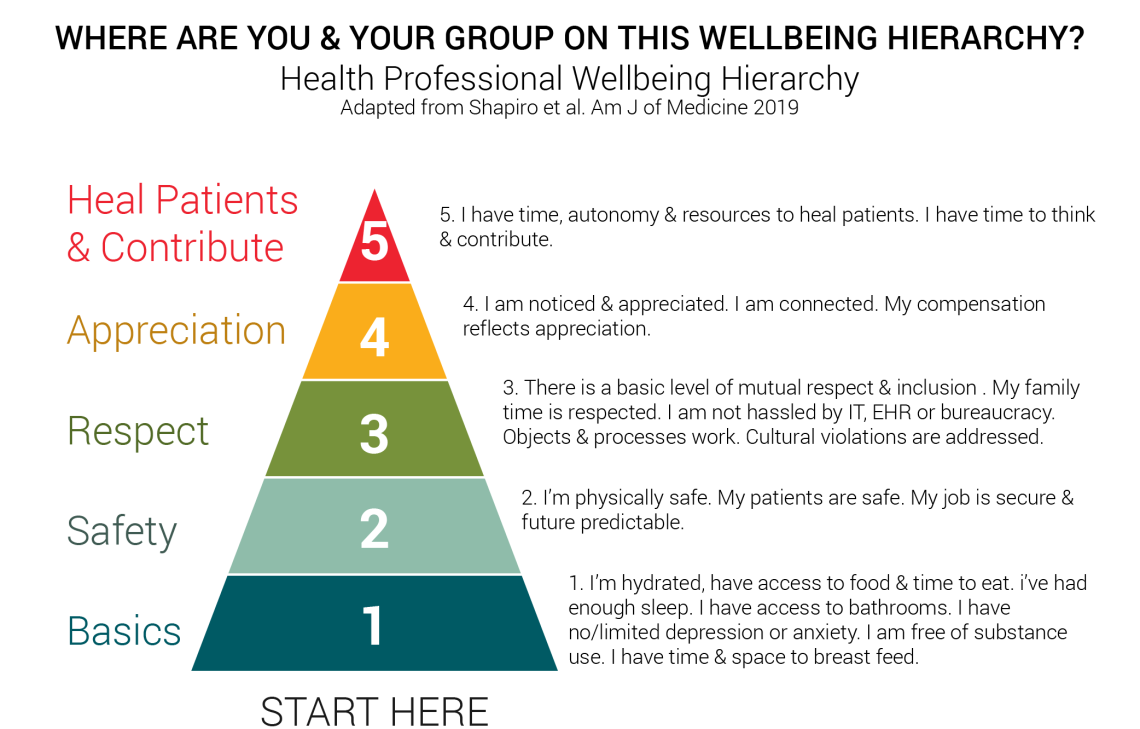
#1: Self-assess by asking “Where are we on the wellbeing hierarchy?”
The Health Professional Wellness Hierarchy provides an easy-to-use framework, drawn from Maslow’s hierarchy of needs, that can help your team self-assess wellbeing needs. As a team, reflect on where you fall. It’s okay to be at a basic level; you’ll most likely struggle to make higher-level changes without first addressing basic needs.
#2: Make it measurable and ask “Do we have data?”
Many people want to start with a survey. While data is great, you probably already have some. Consider which surveys, focus groups, or deep discussions you’ve already had. Talk with Human Resources, the Medical Group, and the Resiliency Center to see what data is available (see resources below). While a survey can be useful, sometimes the best strategy is to have an open conversation with the team about what are the bright spots and what is getting in the way.
#3: Take a moment to consider “What might have the biggest impact?”
When we think of wellbeing we often focus on personal resilience, and for good reason. It’s the area where we, as individuals, have the most control. It’s why the Resiliency Center focuses on equipping all employees, staff or faculty, with tools to help them build their wellbeing.
Yet, experts note that about 80% of resilience is related to system issues. Those issues include cultural ones (like shared values, connection to meaning in work, and psychological safety) as well as operational ones (like the work we ask our teams to do, and the efficiency of our practices).
Take a step back when you are considering where to place your focus. Think about what might make the biggest difference with the least amount of effort. It also helps to assess your strengths and build on them. Working from strengths is likely to be a lighter lift and show results faster.
Once you’ve determined some team-focused areas of improvement, take care to ensure they can be implemented.
Who’s on board?
Improvement efforts are successful when the whole team is involved. Everyone who has a stake in the processes you’re trying to change has to be at the table and part of the discussion. In my experience, the projects that have been most successful involved all groups that will be affected: physicians, MAs, and office staff.
- Identify who will be impacted and get them on board.
- Determine the extent of the improvement work. Is this a department mandate or one person’s pet project? Knowing who is behind this project can help you consider scope (i.e. should this be big or small, target a small or large group of people, etc.)
- Match your project to your resources, and particularly consider time requirements.
- Local leadership support is essential to success. Involve leaders in the conversation early and continue to enlist their support.
How can your team do it?
Determine if similar efforts are already in place. It is easy to think in isolation, but much more effective to build on existing work. Many groups are working on efforts to improve professional wellbeing, some explicitly and some not. Consider efforts designed to address patient satisfaction, clinical efficiency, workplace culture, diversity and equity, and mentorship, among others. Call colleagues and ask what they are doing in these areas.
Find the pebble in your shoe. If you can identify the small things that make big impacts, you may be able to quickly make some big wins while decreasing stress, increasing a feeling of control, and helping to build a culture of wellbeing.
Two successful models include the Mayo Clinic Listen-Act-Develop and University of Utah Wellness Champions. Both use a value-based approach to identify targets impacting wellbeing, develop a plan to address, and continually reassess using a quality lens.
Physician Engagement Model
Actively seek to identify and understand specific burnout drivers.
Empower physicians to develop and implement solutions to address top burnout driver in their work area.
Develop physician leaders in the context of the improvement work.
Commit to continuous cycle of performance improvement.
Set measurable parameters to know when you’re done. To ensure you’re moving the dial, establish accountability and measure impact. If you don’t have any accountability or way to measure your impact, you won’t be able to continuously improve or know if your approach has any impact at all. Your efforts in changing the course of stress and burnout are worth the effort to measure.
You don’t have to go it alone. No matter where you are in the process of taking on team burnout, support is available. Here are a few options:
- Resiliency Center: The Resiliency Center (RC) works with groups to consider wellbeing in a variety of ways.
- Human Resources and Organizational Development: Both Academics and Hospitals Clinics HR teams can assist.
- Office of Health Equity Diversity and Inclusion: Working to create an inclusive climate while addressing health and education inequities within U of U Health.
- Graduate Medical Education Wellness Office: GME Wellness provides a range of services to residents and fellows.
- Academic Affairs: Resources for faculty and students.
- Value Engineering: Access the team of lean six sigma experts to facilitate value improvement work.
- Home for Dinner: Help build provider efficiency and satisfaction with EHR.
Top articles on approaches to systems and teams
-
Shanafelt and Noseworthy, Mayo Clin Proc, Executive Leadership and Physician Well-being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout, 2016.
-
Swensen et al., J Healthcare Management, Physician-Organization Collaboration Reduces Physician Burnout and Promotes Engagement: The Mayo Clinic Experience, 2016.
-
Shapiro et al., Am J Med, Beyond Burnout: A Physician Wellness Hierarchy Designed to Prioritize Interventions at the Systems Level, 2016.
Amy Locke
When life gets busy, it’s easy to forget what keeps us grounded and therefore more satisfied with life. Sydney Ryan reflects on the importance of making time for yourself and prioritizing what is important for you. She explains simple, deliberate actions that have made a difference in her work and her life.
Health care workers experience trauma every day in multiple ways, making it difficult to fully recover. Jake Van Epps shares tips for recovering and supporting your colleagues through these adverse events.
Nurses are notorious for not taking breaks—the culture of their work environment doesn’t make it easy. Katrina Emery, a MICU charge nurse working on her doctor of nursing practice (DNP), sheds light on how to change culture to prioritize breaks to improve health and wellbeing.
