BY THE NUMBERS
U of U Health CVICU local practice patterns between February and December 2017:
- 15,808 ABGs ordered
- Avg. 4.4 per person per day
- 4.7 days avg. length of stay
The problem and scope
Unnecessary tests represent a significant portion of health care’s expense. ICU care accounts for 13% of overall hospital costs. An arterial blood gas (ABG) test assesses the function of a patient’s lungs, and is the most commonly ordered test in the ICU.
The national average is two to six ABGs per patient per day. However, in less than half the cases did the information provided in the ABG result change the course of treatment .
We know from national colleagues that we can reduce unnecessary ABG usage. Changing ordering protocols decreased daily ABG use by 14% . When providers discuss reducing these tests during rounds, ABG use declined 60% . And just by re-educating staff about the importance of reducing costs, ICUs were able to save $87,565 yearly savings .
Could we reduce ABGs here at Utah?
The solution: Have patience. Improvement takes time.
Complex problems are never straightforward. This project taught me patience. Everyone wants people to get better faster, pick up knowledge quicker, or learn concepts more efficiently, but all of that takes time.
We started by going to the gemba where the work is done at U of U Health’s Cardiovascular Intensive Care Unit (CVICU). We asked nurses and respiratory therapists, the experts who do the work, whether we were ordering too much or ordering inappropriately. Using a process map, we broke down the clinical processes that lead to and from ordering an ABG.
THE PROCESS MAP REVEALED FOUR OPPORTUNTIES
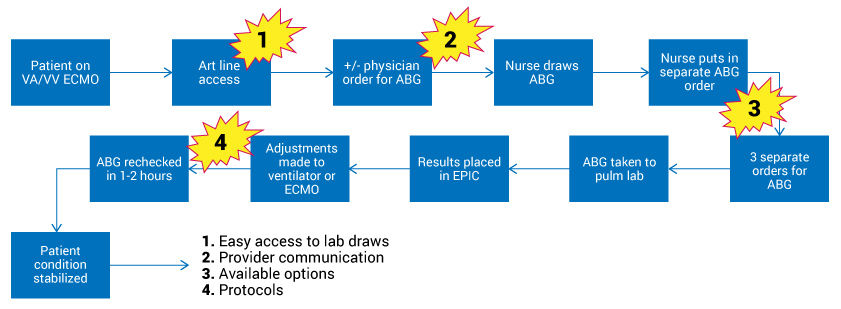
We discovered that ABGs are often ordered because of routine practice, not necessarily because the patient’s condition required it. Nurses ordered ABGs because they thought physicians used the information to make decisions. It turned out that variation existed amongst the physicians and respiratory therapists. Inexperienced physicians didn’t understand why particular ABGs were ordered. It was this run-around where people would say, “Well, we get them because we just get them. We don’t know exactly why we’re using them, but we were told to order them.”
Quality
Refining the existing ABG protocol is an opportunity. Are we ordering the appropriate test for the patient’s condition? If a patient is on ECMO and fairly stable, do we need to order the ABG that contains the most information and costs the most money if we’re not using all of that information? A more specific protocol offers nurses the autonomy to understand which kind of ABG they should order.
Cost
Addressing how Epic prompts providers is an opportunity. We found that the most expensive test was the default provider order.
Culture
Ongoing education to all staff is important. In ICUs, nurses have a lot of autonomy to provide patient care. We have to involve everyone to think critically about whether a test is needed. We as providers can do a better job balancing the individual needs of the patient with appropriate testing. Discussion during rounds is key.
One of the strongest advocates of reducing unnecessary ABGs is the nursing staff. They also thought we were ordering too many tests, but they were under the impression that we needed those tests. By having a conversation with everyone involved in patient care about how and why the labs are utilized, we’ve made a difference.
During a recent night shift when I was caring for a really sick patient, this nurse found me to say, “I know you really care about ABGs. I want to make sure that I have the best strategy. Can we talk about it?” This nurse knew we had been working on the project for the last few months, and it was clear he wanted to join the collaborative process. Right there on the floor, we had a 10-minute conversation about the labs and how we could talk about the results. This example demonstrates how we as a team could better care for our sick patients in the long term. But it was a conversation two years in the making.
What’s next?
We’re starting by targeting extracorporeal life support (ECMO) patients—on average, they receive an ABG test every one to two hours. Our intervention is to change a minimum of three of those to the less expensive test as part of our cost savings. That can make a significant difference.
At the end of the day, reducing unnecessary tests is about culture. It’s easier to get support when you have a relationship with the people doing the work. As care providers, we are all connected, and when we are authentically enthusiastic as a team about improvement, it helps us deliver the best care for the patient.
Like Dr. Seuss says in one of my favorite quotes, “Unless someone like you cares a whole awful lot, nothing is going to get better. It’s not.”
View Riann’s full presentation at the Department of Surgery’s Value Symposium here (from 1:03:30 – 1:14:45).
We learned of Dr. Robbins' improvement work at the second annual Department of Surgery Value Symposium this past July 11. Her project was one of two selected to be profiled on Accelerate. We applaud these efforts to share and spread best practices in delivering high-value health care within our community and beyond
Community Correction: August 27, 2018 - This article has been corrected to reflect 13% of overall hospital costs attributed to ICU care, not individual test. Additionally, the study reflecting re-education of staff was corrected to reflect a $87,565 annual savings.
Riann Robbins
The practice of medicine is recognized as a high-risk, error-prone environment. Anesthesiologist Candice Morrissey and internist and hospitalist Peter Yarbrough help us understand the importance of building a supportive, no-blame culture of safety.
Medical errors often occur due to system failure, not human failure. Hospitalist Kencee Graves helps explain why we need to evaluate medical error from a system standpoint.
In this provocative thought piece, hospitalists and system leaders Kencee Graves and Bob Pendleton explain the “team of teams” approach to becoming more nimble, responsive, and adaptable to the demands of our changing world.
