he worlds we live in can be distilled into three types: simple, complicated, and complex.
A simple world is one in which a single individual can act and trace the effects of those actions. There are no ripple effects. Historically, a doctor, working as a sole practitioner on a house call, worked only with the patient. The doctor diagnosed the patient, prescribed a course of treatment, and that was that.
A complicated world has more moving parts than a simple world, but the ways those parts move, or relate to one another, are discrete and predictable. The insides of a watch are certainly complicated, but once taken apart you can put them back together. Thirty years ago, the hospital was a complicated place, with nurses and physicians and a limited number of other personnel working together. It was complicated because there were more interdependent pieces than the historical doctor-patient model; but, the different parts, like the components in a watch, tended to work over and over again. This was the beginning of the hierarchical health care team and the preferred metaphor was the physician as captain of the ship. We formed, we stormed, we normed, and we performed, under the captain’s direction.
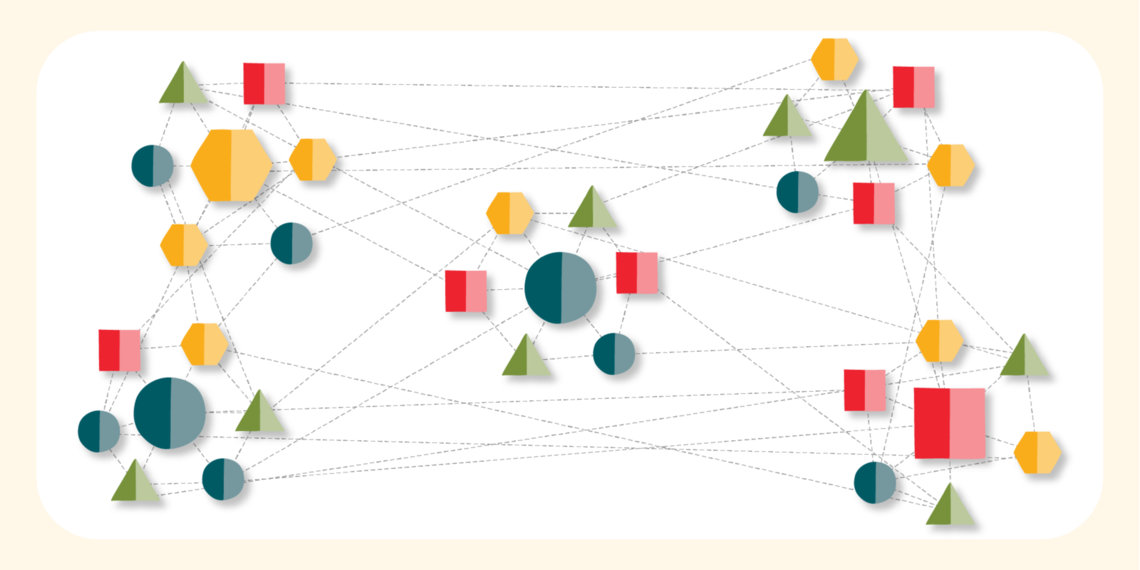
In a complex world, the number of moving parts increases, and how those parts relate to one another also changes. Interactions are unpredictable, surprising, and enormously difficult to understand. And various parts are not even always present in the system. Complex systems are dynamic; they look like biological systems, not mechanical systems. This is the world of health care now: every month, every day, every hour, every minute can look different than the one which preceded it as knowledge changes quickly. In this world, the traditional organizational chart is too rigid for such a fluid practice environment. It takes too long for information and action to move up and down the chain of command, limiting the ability of the system to rapidly adapt to these changing conditions.
A complex world calls for a new way of organizing ourselves.
Organizing for complexity: team of teams
Our system of care is too complex for any one person to be able to sit and map it all out, with others following this command. Instead, we need to open the door to all kinds of dialogue so we can map the interdependencies that will help us get where we want to go as a system. This approach is what Stanley McChrystal has called team of teams. A team of teams requires creating a shared organizational consciousness, which is best described with three parts: vision, guardrails, and empowered execution.
![]()
First, determine your vision, or where you want to go as an organization. At the University of Utah, we have determined that our vision is to be a patient-centered health care organization distinguished by collaboration, excellence, leadership, and respect. These principles allow everyone, from environmental services to nurses to executives understand what we are working toward.
Second, develop principles or guardrails for how to get there. Guardrails can be the rules or policies that are in place. For example, when the University of Utah developed its General InPatient (GIP) hospice program, there were regulations from University of Utah Health as well as from Centers of Medicare & Medicaid Services (CMS) that had to be respected. Otherwise, as long as the program fit within the vision described above, it could be developed.
Third, empower people to make decisions on-demand, rather than waiting for decisions to come from executive leadership. Imagine if every time there was an issue with a dissatisfied patient, we required a decision from executive leadership–it would take far too long for us to deliver high quality patient-centered care.
Lastly, it is helpful to collect and share information. A variety of qualitative and quantitative metrics help you understand whether or not you are making progress toward your vision.
Once everyone understands where you want to go, and understands the ground rules for what you can and cannot do to get there, teams are free to operate nimbly and responsively. The result is a group of people who are empowered to move and adapt fluidly, within their own spheres and as their own teams, without having to run every decision through the C-suite.
An organization that operates under a team of teams model is distributed (or networked), flexible, and agile.
How our approach changes who we are
What does this organizational approach mean for our organization? We are already well on our way.
Approaches to recruiting and accountability might change. Right now, U of U Health hires people who have an intense amount of individual accountability. It is a method that has brought us tremendous organizational success. We’ve recruited individuals who feel responsible and accountable for moving things forward. We’ve rewarded people who have the transactional ability to get from A to B. But in a team of teams model, that changes. In this complex world, we have to find the interdependent people and work with them in a relational way, and not in a transactional way, to develop solutions so that all of these interdependent pieces are working together.
There is some good news here, because while that may seem complicated—or complex—it is fun. Approaching our peers and teams relationally, rather than transactionally (that is, as people we work with, rather than as people we work through), is immensely rewarding. As an organization, we already do much of this naturally.
We are a collaborative organization. We hire genuine people and we promote a culture of respect. Moving toward a team of teams approach isn't a wholesale change, rather a continued investment in who we are. Moving forward in this journey, we have an opportunity to deepen our respect for relationships and our natural desire to overcome silos. Doing so will help us learn new ways to work and deliver care to maintain our collective success.
Interested in a deeper dive with Bob and Kencee? Check out:
-
Team of teams: New rules of engagement for a complex world, Stanley McChrystal
-
Overcomplicated, Samuel Arbesman
-
Health care as a complex adaptive system: Implications for design and management, William B. Rouse
Kencee Graves
Bob Pendleton
What is the strongest predictor of an effective solution? It’s not the size of the committee or the length of the brainstorming session. The best predictor of successful solutions is how well the problem is understood. Investing time in defining, investigating and analyzing the problem can lead to transformative solutions.
Improving value in healthcare means redesigning care to meet patients’ needs. We must push ourselves beyond patient satisfaction surveys to reduce uncertainty, complexity, and confusion in the delivery of care. Matthew Stein, MD, and the Breast Imaging team unflinchingly faced a source of uncertainty for patients: waiting for mammogram results.
The following case study examines a new core competency in delivering value at a system level. At the University of Utah, leaders created integrated oncology teams organized for the patient. Collapsing historical silos and empowering front-line leaders grew adaptive teams that offered better value to cancer patients.