takes more than the knowledge acquired through education and training to be a truly exceptional clinician. Even though you will spend an extraordinary amount of time becoming an expert in your area of study, some effort spent on building relationships will help you strike an ideal balance.
Relationship management skills are sometimes referred to as “soft skills” or non-technical skills, which may minimize their importance. Using acquired skills and knowledge, while also understanding the science of relationship building, allows each individual clinician to effectively promote cooperation and trust among their teams, to empower them to improve patient outcomes.
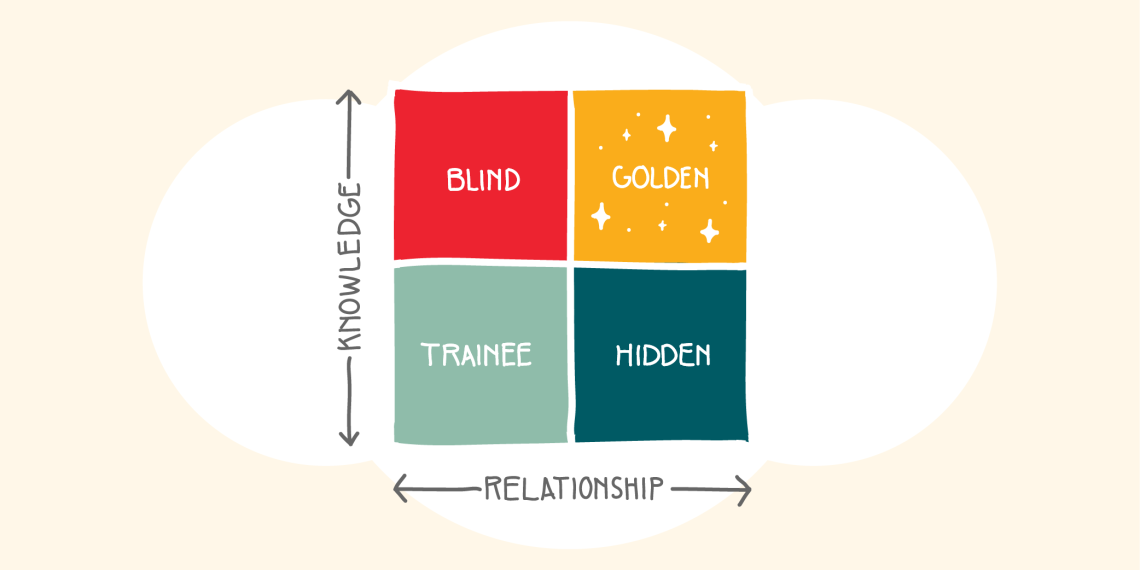
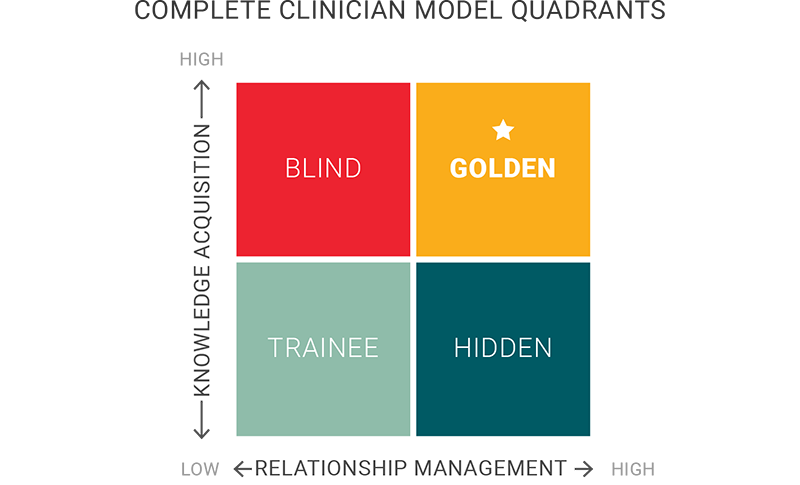
The complete clinician model quadrants
In thinking about the two components of clinical excellence—relationship management (RM) and knowledge acquisition (KA)—it may be helpful to put them each on an axis of a 2x2 table. On one axis is the development of relationship skills, and on the other is the acquisition of knowledge essential to provide a good clinical outcome. Everyone begins in the bottom left square as a trainee. As you progress through training and clinical experience, you should be working on achieving high levels of clinical knowledge and high levels of relationship management to reach the “golden” quadrant in the top right.
However, it’s not always a straightforward path to get to the golden quadrant. It requires focused effort to build both types of skills.
Trainee quadrant
The trainee quadrant is where we all start. It's not bad to be in this quadrant, but our goal is to get to the golden quadrant by acquiring knowledge and learning how to form excellent relationships. A trainee’s efforts are often centered around learning basic science and clinical treatment concepts. It's critical to develop knowledge of exceptional and clinically sound treatment for patients. But it’s important not to get so caught up in KA and neglect the development of RM skills.
Ideally your progression through the trainee quadrant is diagonally up toward the golden quadrant, rather than straight up (toward the blind quadrant) or straight across (toward the hidden quadrant). Different people develop different skills at different levels, so it’s okay if yours are not always a perfectly balanced or linear path.
Blind quadrant
Those in the blind quadrant are smart and skilled, but perhaps lack insight into how their behavior affects others. Someone who falls into this quadrant understands clinical care exceptionally well and can provide great recommendations on the best course of treatment or the latest research. However, they may lack the interpersonal skills necessary to connect with both patients and peers. This can significantly impact a clinical team and contribute to dysfunction if not addressed.
Hidden quadrant
Those in the hidden quadrant are wonderfully collaborative, but are perhaps not trusted, because of their lack of skill and knowledge. This can be particularly dangerous for patient care, as the person might be exceptionally well-liked, but may not be able to determine the best treatment. Highly developed RM skills may also mask clinical inadequacies. When people work with a friendly and collaborative clinician who they like on a personal level, they might be less likely to question that person’s skills. This can put patients at higher risk of suffering from malpractice or clinical negligence.
Golden quadrant
In the golden quadrant, clinicians have learned relationship management skills with patients, caregivers, colleagues, and multi-disciplinary team members. This is the ideal balance; you have the right skills to identify proper care for a patient, as well as the ability to build collaboration and consensus among team members. In addition to being well-liked by patients, clinicians in the golden quadrant effectively foster trust and collaboration among team members, improving outcomes for all patients while contributing to a highly collaborative work environment.
Barriers and catalysts
Unfortunately, there are barriers that can prevent a team or individual from getting to the golden quadrant. These include:
-
Psychological distress—an environment where team members do not feel safe to take risks, speak up, or ask questions.
-
Incivility and intimidation—behaviors that lead to power differentials and make it impossible to build consensus and collaborate effectively.
-
Vulnerability—at the extreme, vulnerability can lead to fear that brings out uncertainty in team members and increases the perceived emotional risk of speaking out or taking action.
- Abuse—the most extreme barrier that will destroy a team. Abuse can take many forms: physical, emotional, psychological, financial, bullying, and harassment.
Not to be overlooked, there are catalysts that help people develop the right balance of clinical skills and knowledge. By developing team psychological safety, obtaining feedback, learning to disagree without being disagreeable, improving teamwork culture, and even showing appropriate vulnerability, individuals and teams can promote golden quadrant tendencies.
Each of these things can be discussed and promoted by your teams to get them to the golden quadrant. As golden individuals maintain the dual focus of knowledge acquisition and relationship management, they will have an objective in mind, discuss and interact with other experienced team members and make decisions based on the best information. Thus, health care challenges will be met with innovation and excellence. As golden teams maintain the same dual focus, they will solve health care challenges in amazing ways.
We will further explore barriers and catalysts to training and the Golden Quadrant domains in future Accelerate articles, so stay tuned!
Resource:
Jared W. Henricksen, Deirdre Caplin, Joni Hemond, Kyle M. Turner & Connie Madden (2020) The complete clinician model, Baylor University Medical Center Proceedings, 33:3, 492-496, DOI: 10.1080/08998280.2020.1763137
Deirdre Caplin
Joni Hemond
Jared Henricksen
Performing a rapid critical appraisal helps evaluate a study for its worth by ensuring validity, meaningful data, and significance to the patient. Contributors Barb Wilson, Mary Jean Austria, and Tallie Casucci share a checklist of questions to complete a rapid critical appraisal efficiently and effectively.
Quantitative and qualitative methods are the engine behind evidence-based knowledge. Tallie Casucci, Gigi Austria, and Barbara Wilson provide a basic overview of how to differentiate between the two.
Medical students Rachel Tsolinas and Sam Wilkinson, along with SOM professor Kathryn Moore, share a practical tool all health care professionals can use to broaden our understanding of how culture influences decisions and events.