The Challenge
very chemotherapy treatment requires orchestrated teamwork: the physician who orders chemotherapy, the pharmacist who prepares the medication, and the nurses who administer it to the patient. What could be chaos—many people participating in the process, complex medication regimens, scared and anxious patients—felt organized (most of the time) to the patient. Our team at Huntsman decided that wasn’t enough. Every patient, no matter where they receive care the University of Utah system, deserves safe, standardized care.
The Problem and Scope
Redesigning workflow so patients feel safe
Patients undergo chemotherapy at University of Utah’s Huntsman Cancer Institute, but they can also receive chemotherapy treatments at two Huntsman satellite community clinics in the University of Utah Health system. It's common that a patient will receive chemotherapy at HCI’s main infusion center on one day and at the clinic closest to their home on a different day.
The problem was that everyone was doing things a little differently. From a patient’s perspective, even little differences create anxiety. If you see one nurse giving your chemotherapy one way, and the other doing it slightly different, you might be nervous that someone is doing it wrong. The difference might not be meaningful, but patients don’t know that.
We also wanted to ensure that we're following national standards. It's easy to take shortcuts because we’re all busy, but shortcuts can lead to mistakes. There are studies that show that when you do a process every day, it's easy to convince yourself that you’re following protocol, but you may not be.
Use technology to error-proof the change
A few years ago, University of Utah integrated most intravenous pumps with our electronic medical record, Epic. Pumps are used throughout the inpatient units to deliver medications and fluid to patients. Connecting the pumps with Epic means less manual work (and less chance for errors) to calculate the correct amount of fluid or medication for a patient.
Pump integration had not worked well with chemotherapy because of how chemotherapy is administered. Chemotherapy is ordered by volume, not hourly like most other IV medicines or liquids. We have to know the exact volume of the chemo bags in order to set the correct rate, because the entire bag is needed to treat the patient. Intravenous bags come to us from the manufacturer with inexact volumes–sometimes slightly underfilled, sometimes slightly overfilled. Pump integration hadn’t worked with chemo because of this volume discrepancy and to solve it meant big process changes for pharmacy. We took this opportunity to make changes to both nursing and pharmacy workflows.
The Solution
Build an interdisciplinary team to create broad understanding
We started about two years ago with a committee led by Melissa Banner, former nurse manager of the 4th floor inpatient unit at Huntsman Cancer Hospital. Our committee included inpatient nurses, nurse managers, educators, pharmacy, nursing informatics and IT. Pharmacy director Scotty Silverstein and pharmacy manager William Black were necessary members–we wouldn’t have been able to do this project without them. Pharmacy is very safety conscious, but we needed to work together to understand issues and workflows.
Having frontline staff was important for buy in. We knew we couldn’t just tell people what was going to change, we needed their buy-in. Chemotherapy administration is a high risk procedure and luckily we don't make many mistakes. But, if a mistake happens, it can be devastating for the nurse and the patient. Our purpose was to change the process to come close to eliminating any chance of error. Over the years, we had tried lots of different ways of changing practice, but it hadn’t worked. I think by saying, "This is how we're all going do it, we're all in the same boat," I think that made the difference.
Dual-check Protocol
Nurses use pocket reference cards as reminder of their checklist.
- View inpatient pocket card.
- View outpatient pocket card.
Standardize the process and use a checklist
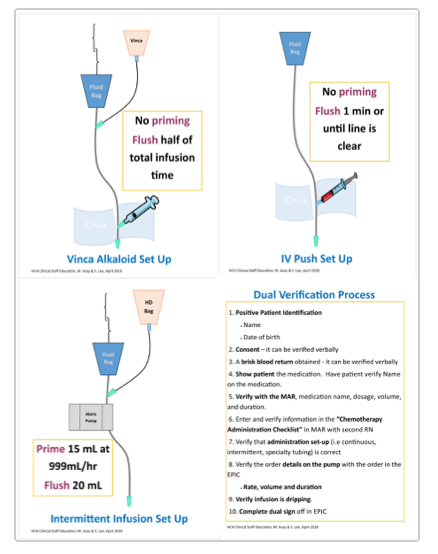
We researched national best practices, including specifics like how the supplies and tubing are laid out. We wanted to set up the tubing the same for every kind of infusion, whether it was piggy back or continuous. We wanted to manage the flushing the same way.
We established a bedside dual-check protocol. The patient’s nurse sets up the chemotherapy, and then another nurse comes to sign off on their work. The second nurse ensures everything is connected–the line is dripping correctly and not dripping on the floor. There are all these little steps but it literally takes seconds. The big difficulty is trying to get two nurses together in infusion because they're busy. We had always had a dual check, but it wasn't at the chair or bedside. Now, because nurses are also checking the medication rate on the pump, there is only one spot to do the check: at the bedside.
Integrate technology
One of the main errors in chemotherapy is a medication error where a patient is given too much medication too quickly. You need the right amount of drug given at the correct rate. Being able to use technology that existed, like pump integration with the EMR, would allow us to improve safety around these types of potential errors. This solution took work to update the pump drug library, make required changes in Epic, and revise nursing and pharmacy practice.
Other organizations have used work arounds that required a nurse to manually re-program the pumps. Because our pharmacy team were deeply involved, we were able to avoid this time-consuming (and error-prone) task. The pharmacy team now weighs all chemotherapy bags and removes excess volume to equal the ordered volume. This step allows pump integration to work as intended with no re-programming needed.
The nursing informatics team worked to integrate pumps with Epic across the U of U Health system, and clinical staff education (CSE) developed learning for all staff. The new process reduces the nurse’s manual work by automating the pump rate calculation.
Now, patients are connected to the pump through an IV or port. The nurse opens the medication record, scans the drug, scans the patient, and then Epic sends the order to the pump wirelessly, so the nurse doesn't have to do any programming of the pump. The nurse can also "stop the line" by halting the process at any time if they believe there is an error.
Lessons Learned
The power of a diverse team
Having a big group with representation from all of those areas (nursing, IT, pharmacy, educators, leaders) allowed us to get this done. Everyone had a voice, everyone felt like they were a contributor. We’re all concerned about the quality and safety we’re giving our patients, so we all supported this process.
The power of auditing
Our educator team was critical to our success. To implement the new protocols, we needed a lot of education. Clinical Staff Education (CSE) provided education around pump integration; Gigi Austria’s team supported us on education for chemo standardization. Infusion and inpatient-focused educators Marie Asay and Sunghee Lee were our key educators. They developed training modules, knowledge assessments, and skill competency verification. They did one-on-one training with every single nurse who administers chemotherapy throughout the entire U of U Health system–about 140 nurses.
Even with our excellent education and training, I know that we are not doing it every time because we’re human. Nurses will say "Well, I've done this for a long time I'm not going to make a mistake." We like to think that if we do something enough, we're really good at it. That’s not true. Our mind and our hands are not always perfectly in tune.
Be Aware of Bias
Cognitive biases affect all of us. Being aware of the biases that affect our decision making and implementing best practices, such as checklists and dual checks, supports staff by reducing individual blame and fostering a safety culture.
More articles on addressing bias in health care:
One of the things that I've tried to teach my staff is, "We're all fallible. We're humans so we make mistakes. We’ve created standardization to prevent mistakes." That's why pilots go through a checklist before they take off and even though they've done it for 20 years, they still have to do that physical checklist. Chemotherapy double checks are the same thing. A few years ago I read Dr. Atul Gawande's The Checklist Manifesto and it was a big influence in how I approached this issue.
We’re deliberately hardwiring the process through continual audits and yearly competency testing. Every nurse has a visual audit every six months. If someone doesn’t follow the appropriate steps or pass a competency test, there is remediation.
Results
Poster Presentations
Implementation of Pump Integration and Administration Standardization of Chemotherapy Across a System (Accepted: Oncology Nursing Society)
To measure our success and add individual accountability, we look at monthly pump compliance reports and break out results by unit and by individual RN. In FY19, we set a goal of 95% compliance for outpatient staff and had great results. For example, Bone Marrow Transplant infusion staff in 3rd quarter were at 97% as a group and all RNs met or exceeded the 95% goal.
So far, we've seen a reduction in safety reports in our RL system as well. In FY18, there were 5 chemotherapy administration issue reports, and only 2 in FY19.
Our team recently talked about our unfinished business and what’s next. With USP800 coming soon, there are many more safe handling issues that we’ll need to address. We’re segueing into those issues, and this diverse team will allow us to work on it together.
Joy Lombardi
The practice of medicine is recognized as a high-risk, error-prone environment. Anesthesiologist Candice Morrissey and internist and hospitalist Peter Yarbrough help us understand the importance of building a supportive, no-blame culture of safety.
Is zero possible? In the case of central line infections, the answer was once no. A CLABSI (central line associated blood stream infection) was once considered a car crash, or an expected inevitability of care. When University of Utah’s Burn Trauma Intensive Care Unit started treating CLABSIs like a plane crash, or a tragedy demanding in-depth investigation and cultural change, zero became possible.
Your gut tells you a process could be better than it is—how do you back that feeling up with hard data? Senior value engineer Luca Boi shows how undertaking a baseline analysis can jumpstart your improvement project.
