Learning Objectives
After completing this lesson you will be able to:
(1) Define evidence-based practice (EBP)
(2) Describe the role of research and EBP in clinical practice
(3) Discuss the differences between research and EBP
Case Study
Shay is a clinical nurse on the Bone Marrow Transplant & Hematology Inpatient Unit. She is assigned four patients, three of which have multiple blood products ordered. Throughout the day, Shay notices the Health Care Assistant (HCA) is “frazzled,” running from room to room to obtain frequent vital signs on these patients. A fall-risk patient in room 25 hits their call light to ask for help to the restroom, but the HCA is busy in room 31 with more vital signs. The patient decides to get up without assistance, and falls. Shay starts to wonder, “Is there a better way to do this?” She also realizes that she has never personally seen a blood transfusion reaction happen on the unit, and asks herself, “How often do transfusion reactions actually happen? Does the evidence support vital signs being done this frequently?”
What is evidence-based practice?
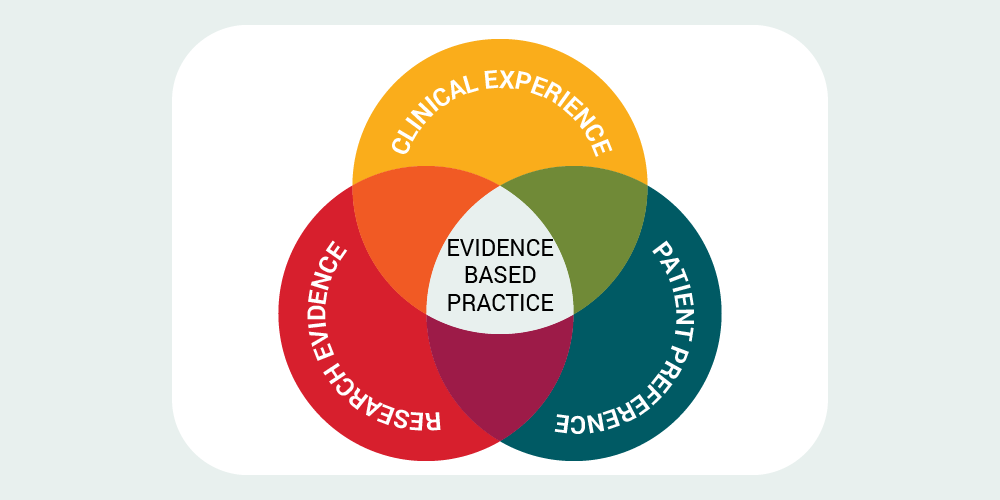
videnced-based practice (EBP) is applying or translating research findings in our daily patient care practices and clinical decision-making.
EBP also involves integrating the best available evidence with clinical knowledge and expertise, while considering patients’ unique needs and personal preferences. If used consistently, optimal patient outcomes are more likely to be achieved.
Using EBP means abandoning outdated care delivery practices and choosing effective, scientifically validated methods to meet individual patient needs. Health care providers who use EBP must be skilled at discerning the value of research for their specific patient population.
How to apply EBP in clinical practice
Evaluating all of the available evidence on a subject would be a nearly impossible task. Luckily, there are a number of EBP processes that have been developed to help health care providers implement EBP in the workplace.
The most common process follows these six steps:
1. ASK a question. Is there something in your clinical setting that you are wondering about? Perhaps you wonder if a new intervention is more effective than the one currently used. Ask yourself: What works well and what could be improved? And, more importantly, WHY? Evaluate the processes and workflow that impact, or are impacted by, the identified practice gap. We’ll use a format called PICO(T) (pronounced “pee ko”). Learn more about PICOT questions in the next module.
2. ACQUIRE the current evidence. You’ll do this by conducting a literature search. Your search will be guided by your clinical question.
3. APPRAISE the literature. Or, in other words, sort, read, and critique peer-reviewed literature.
4. APPLY your findings to clinical decision-making. Integrate the evidence with clinical expertise and patient preferences and values. Then make evidence-based recommendations for day-to-day practice.
5. EVALUATE your outcomes. Review data and document your approach. Be sure to include any revisions or changes. Keep close tabs on the outcomes of your intervention. Evaluate and summarize the outcome.
6. DISSEMINATE the information. Share the results of your project with others. Sharing helps promote best practices and prevent duplicative work. It also adds to the existing resources that support or oppose the practice.
Though we may learn how to apply EBP by participating in project-based work, integrating EBP in our daily practice can help us strive to achieve the best possible patient outcomes. It requires us to be thoughtful about our practice and ask the right questions.
It's important to note that although applying evidence at the bedside can be conducted individually, working collaboratively as a team is more likely to result in lasting improvement.
Before there was evidence…
As health care providers, delivery of patient care should stimulate questions about the evidence behind our daily practice.
For instance, there was a time when neutropenic patients were placed in strict isolation to protect them from developing life-threatening infections. Research findings were evaluated for best evidence and it was noted that using strict isolation precautions did not result in more favorable patient outcomes when compared to proper handwashing procedures coupled with standard precautions—and it seemed that we unnecessarily subjected patients to the negative psychological effects caused by extreme isolation.
As clinicians, we sometimes follow outdated policies or practices without questioning their relevance, accuracy, or the evidence that supports their continued use.
What’s the difference between research and EBP?
There is a common misconception that EBP and research are one in the same. Not true! While there are similarities, one of the fundamental differences lies in their purpose. The purpose of conducting research is to generate new knowledge or to validate existing knowledge based on a theory. Research involves systematic, scientific inquiry to answer specific questions or test hypotheses using disciplined, rigorous methods. For research results to be considered reliable and valid, researchers must use the scientific methods in orderly, sequential steps.
| Research | Evidence-based Practice |
|---|---|
| To generate new knowledge or validate existing knowledge based on theory. | To use best available evidence to make informed patient-care decisions. |
In contrast, the purpose of EBP isn’t about developing new knowledge or validating existing knowledge—it’s about translating the evidence and applying it to clinical practice and decision-making. The purpose of EBP is to use the best available evidence to make informed patient-care decisions. Most of the best evidence stems from research, but EBP goes beyond research and includes the clinical expertise of the clinician and healthcare teams, as well as patient preferences and values.
Before you begin – a few important considerations
Do you have more than just evidence?
Patient Feedback

Need help getting patient feedback? Learn about U of U Health's Patient Design Studio.
Research findings, in the absence of other considerations, should not be used independently to justify a change in practice. Other factors that must be considered include:
-
Patient values and preferences
-
Experience of the health care provider
-
Patient assessment and laboratory findings
-
Data obtained from other sources, such as unit-based metrics and workflow
For EBP strategies to result in the best patient outcomes, all of these factors must be considered.
Do you have adequate sponsorship and resources?
Start Smart

For more helpful tips to get started, read "Ask These Four Questions Before Starting Any Improvement."
To implement EBP, we also need to consider if the implementation of the project will be supported by administration and institutional resources. For example, suppose there is a strong body of evidence showing reduced incidence of depression in pregnant women who receive cognitive therapy sessions when they are hospitalized for extended periods of time. While this might be a great idea, budget constraints may prevent hiring a therapist to offer this treatment.
While you are thinking of resources, think about people, or human resources. Who in your organization can assist you with the project? Are there content experts or key stakeholders that you should involve early on?
Do you have access to data and a plan for measuring progress?
Just like research, we must evaluate and monitor any changes in outcomes after implementing an EBP project so that positive effects are supported and negative effects are remedied. An intervention may be highly effective in a rigorously controlled trial, but that doesn’t always indicate it will work exactly the same way in your clinical setting or for your individual patients.
Conclusion
The goal of conducting EBP is to utilize current knowledge and connect it with patient preferences and clinical expertise to standardize and improve care processes and, ultimately, patient outcomes.
Resources to get started:
- Contact the Evidence-based Practice Council (U of U Health) An interprofessional collective dedicated to incorporating evidence-based practice into daily work.
- Clinical Skills: Clinical Staff Education (U of U Health) The “Clinical Skills” tab offers a host of evidence-based practice changes to start applying today.
- Eccles Health Sciences Library Resources (EHSL U of U Health) Resources, tips, and tools for evidence-based practice in health care.
This article originally appeared 12/18/19. It was updated to reflect currrent practice 2/26/21.
Barbara Wilson
Mary-Jean (Gigi) Austria
You have a good idea about what you want to study, compare, understand or change. But where do you go from there? First, you need to be clear about exactly what it is you want to find out. In other words, what question are you attempting to answer? Librarian Tallie Casucci and nursing leaders Gigi Austria and Barb Wilson help us understand how to formulate searchable, answerable questions using the PICO(T) framework.
Librarian Tallie Casucci and college of nursing leader Barb Wilson review the steps to conduct a literature search, as well as provide some local resources to help if you get stuck.
The practice of medicine is recognized as a high-risk, error-prone environment. Anesthesiologist Candice Morrissey and internist and hospitalist Peter Yarbrough help us understand the importance of building a supportive, no-blame culture of safety.