Quick Tips
Tools for teams: Download the assessment (1-page), or use these slides at your next team meeting.
we reach the one-year mark from when our pandemic response began, we find ourselves in what the Substance Abuse and Mental Health Services Administration calls the “anniversary reaction.” SAMHSA’s Phases of Disaster graph is a helpful way to describe the different responses to a disaster as time passes.
We aren’t all necessarily in the same place. Some individuals and groups within our institution and community may be closer to the “reconstruction phase”—a new beginning. Others may feel distant from that. No matter what your experience with the pandemic has been, it has value.
Finding yourself on the curve
While the SAMHSA graph provides a big picture of phases over time, it’s important that we continue to acknowledge that we are experiencing this pandemic differently every day, at both the individual and team level, so that we can better connect to each other and to resources of support. That’s where a tool adapted from the Colorado Healthcare Ethics Resource comes in handy.
The Assess Your Stress tool is a great way to identify where you are on the stress continuum—and what to do about it.
There are four different stages on the stress continuum: thriving, surviving, struggling, and crisis.
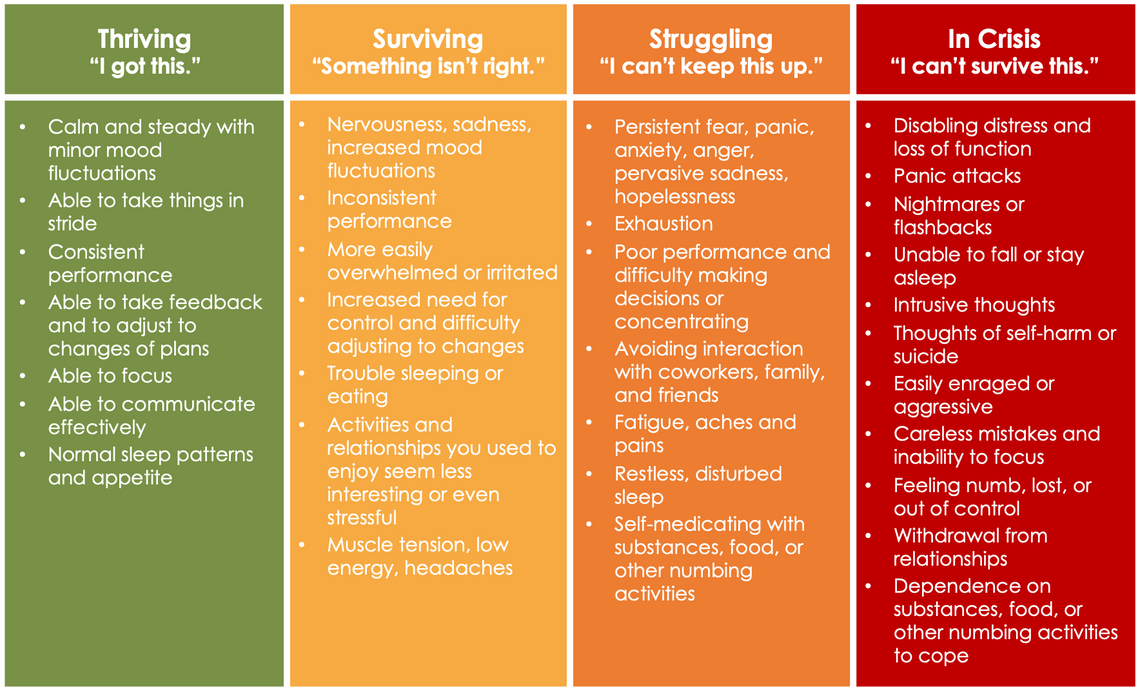
Notice when we are thriving, we are able to have a range of emotions and experiences, we can be happy or sad, energized or tired. We are able to take things in stride and learn and grow. As we move along the continuum toward crisis, our emotions and experiences narrow, usually toward a feeling of being overwhelmed or even numb.
Where are you on the continuum?
Research has demonstrated that naming our feelings can have a strong positive effect on our brains. The term for this process is called affect labeling, or “name it to tame it.”
Take this moment to pause and reflect, asking yourself these questions: Where am I today? Which stage describes me right now?
With this simple self-awareness you can make choices to get your needs met, prevent symptoms from worsening, and engage in practical ways to bounce back.
From identification to action
Now that you’ve determined where you are on the stress continuum, it’s time to figure out what is next. The “Now What” section has simple action items for each stage.
Look at the section that correlates with your earlier response for suggested actions. For example, if you are surviving, you might try to leave some of your to-do list items for another time.
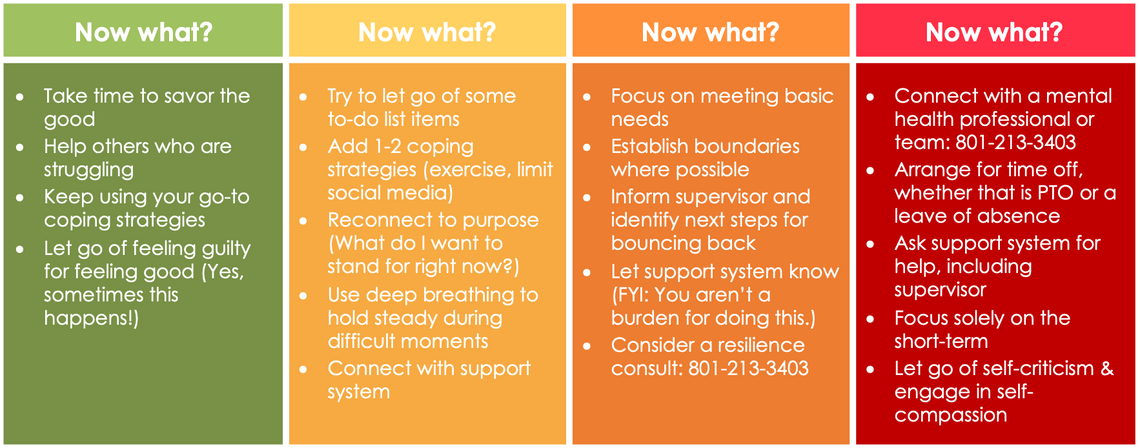
Decide which action item will be most helpful for you today and commit to doing it today. If you can’t commit, ask yourself what support you need to make that one thing happen. The answer might be support from your home environment, from your team, or even permission to practice self-care.
You don’t have to go it alone
At any stage, you can reach out for support. One option is to contact The Resiliency Center. You can schedule a team consultation for a one-hour meeting that provides support and validation and creates a space to learn new skills or talk about next steps.
Tools for teams
Use these slides or play this video at your next team meeting to review this tool as a team.
Discussion questions:
-
How might understanding the stress continuum help us as individuals?
-
How can we use this tool as a team?
-
What stage do we think we are at as a group?
-
What are some ideas we can use from this practice to respond with care as a team?
When discussing as a group, don’t require that individuals reveal the stage they are in. But individuals may volunteer this information if they choose. Also, many may describe that they feel they are in multiple stages throughout the day or week. That’s normal and doesn’t need to be explained or fixed. Some will be drawn to the color of the stages while others will be drawn to the word. Both can represent our experiences.
The most important thing to remember is that pausing to reflect and label what we feel will help us better understand our own needs and the needs of others.
Megan Jean Whitlock
Nurses are notorious for not taking breaks—the culture of their work environment doesn’t make it easy. Katrina Emery, a MICU charge nurse working on her doctor of nursing practice (DNP), sheds light on how to change culture to prioritize breaks to improve health and wellbeing.
When life gets busy, it’s easy to forget what keeps us grounded and therefore more satisfied with life. Sydney Ryan reflects on the importance of making time for yourself and prioritizing what is important for you. She explains simple, deliberate actions that have made a difference in her work and her life.
COVID-19 and social unrest have brought about heightened stress and trauma for our health care community. Nurse manager Bernice Tenort provides a simple exercise to help employees and teams pause, think critically, and respond compassionately when stress levels increase.