Why Value Training?

The Bobcast with Brigitte Smith
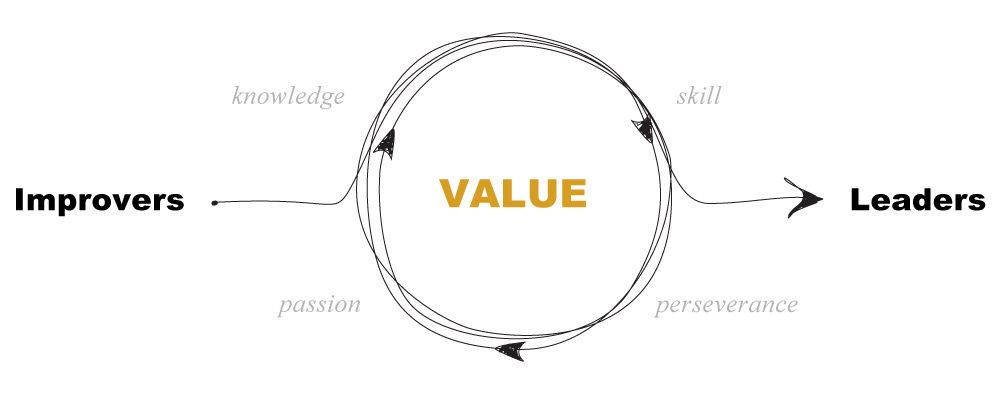
In case you missed it, here's the "why" behind a trainee culture shift for value.
rainees lead improvement efforts throughout our system, and this year the Department of Surgery is recognizing their work at a Value Symposium on July 12, 7:30 – 11:30 at the Huntsman Cancer Institute Eccles auditorium. Teams from five surgery divisions will be presenting their projects, ranging from quality initiatives in Ghana to improving lab usage in Utah’s surgical ICU.
The Accelerate team sat down with Dr. Brigitte Smith to find out how she engages residents in improvement training. The following is a brief excerpt from that interview.
The importance of teaching a skill
I wanted to teach the surgical residents how to lead improvement. Traditionally, resident training in QI has included development of evidence-based protocols for patient care. While a protocol may be one intervention to improve or standardize a process, creating a protocol misses many of the core principles of quality and process improvement. The program director (Dr. Dan Vargo) recognized that the residents needed more rigorous education in order to understand and lead improvement. So we developed the value improvement curriculum to teach the skills required to successfully conduct and lead improvement work.
Initially, feedback from the residents was that the requirement to do a quality improvement project was just more work added to their already endless to-do list. Over time, residents became more engaged as they saw I had a structured curriculum and that I wanted to teach them how to lead improvement. They were learning a valuable, portable skill.
Recognizing the right skills
Improving care delivery starts with deeply understanding the problem, and that’s often hard for physicians. A big part of being a good surgeon is being able to make rapid decisions with incomplete data. You might not know everything about the situation, but the patient in front of you needs something done. As a surgeon, you're trained to have a quick-thinking and decisive mentality. That mentality translates to the way we approach problem solving of systems issues in our clinical environment. You may see that there's a problem with on-time starts in your clinic or over-utilization of arterial blood gas in the ICU, and you're trained to just fix it without stepping back to investigate.
One thing we focused on residents learning this year—do not to start with solutions. That’s why a lot of the projects at the value symposium are still unfinished. Many residents started with the idea, "I will just implement a protocol. I know what a solution could be because I read the literature and I know what someone else did about this problem. I'm just going to implement this thing to fix this problem." Part way through the year, they realized, "Oh, I don't have enough metrics to know if there's a problem at all." Or, they realized "Oh, we started with this solution and now we're realizing that this doesn't really fit the process here at Utah." The ability to really dig into the problem requires process knowledge and skills.
Even though the work is incomplete, it’s really important that it’s shared. We need to recognize residents for learning a new way of approaching problems, and that we don’t only recognize them for implementing some golden solution. The residents have worked hard to learn this new skill. That’s extremely valuable.
I remember being a resident. It's still crystal clear to me how busy they are, with 80+ hours a week of patient care and learning to operate and be a good technical surgeon. As they get more senior, they realize that they can be the best technical surgeon and medical provider there is, but if they don't understand how to deliver that care in the complex healthcare environment, they will not be successful as providers.
Value improvement is a tremendous skill. By sharing their hard work and recognizing their progress, we’re helping to make valuable work visible.
Brigitte Smith
The practice of medicine is recognized as a high-risk, error-prone environment. Anesthesiologist Candice Morrissey and internist and hospitalist Peter Yarbrough help us understand the importance of building a supportive, no-blame culture of safety.
Medical education is steeped in tradition and hierarchy. A new generation of education leaders is sifting through their own stories and experiences to change how students are trained. In this essay, Michelle Hofmann, former associate professor in the Pediatrics department, reflects on her own experience in medical education: a journey from Doctor to Michelle.
Empathy is our cognitive ability to understand, communicate, and respond to another person’s perspectives, experiences, and concerns. Pediatrician Diane Liu reflects on the very real challenges of nurturing empathy in the face of the relentless demands of practice.