arly diagnosis and rapid treatment are key to surviving sepsis, a life-threatening infection that can kill within 48 hours. Previous work done by Devin Horton and Kencee Graves updated Utah’s sepsis protocol with an addition to Epic: a modified early warning system (mEWS) for sepsis that fires an alert and triggers a cascade of actions.
The Emergency Department (ED) recently adapted that work to the fast-paced and critical emergency medicine environment. But the nature of the ED is different than acute care or intensive care units, and the ED team found that the mEWS tools that triggered rapid response on an inpatient unit would not work in the ED.
Accelerate’s Mari Ransco and Nick McGregor sat down with Value Engineer Matt Sanford and the ED’s Jamie Troyer (pictured above left) and Emilie Johnson (above right) to find out how they designed an improvement unique to their culture.
Use the Checklist
Want to adapt the checklist for your team? Download it now.
Our checklist, based on Surviving Sepsis Campaign guidelines, starts at triage and follows the patient through the ED. It identifies key vitals to track, symptoms of severe sepsis, steps to take if concern for sepsis exists, and the process for initiating a Code Sepsis.
Don’t wait for technology
When we started working with Devin and Kencee, we realized that relying on mEWS alone to identify sepsis wouldn’t work. A patient suffering from COPD can present with a high mEWS score but not have sepsis. Someone experiencing an overdose or an asthma exacerbation can present with a high mEWS score but not have sepsis. We had to do something different.
First, we developed a process map reflecting the patient’s journey through the ED. Our working group—Horton and Graves, emergency medicine doctor Christy Hopkins, value engineer Matt Sanford, and nurse practitioner Jessica Singer—got together and tried to apply an algorithm for delivering care in the ED. But when a busy nurse has 20 people in the waiting room, relying on an algorithm doesn’t work. We needed something that would give us a more immediate way to identify sepsis.
Instead, we developed a sepsis checklist, working with Devin to transform the algorithm and revising it several times with Christy Hopkins. We asked IT to do an Epic build with the checklist, but we didn’t have time to wait. So we created a paper checklist. We weren’t trying to go back in time by using a physical piece of paper—we just needed an immediate solution.
The power of checklists
Nurses (and everyone else) love checklists. That’s the way our brains are built. We’re very protocol-driven—especially in the ED, where we have to know so much about so many things. This checklist is easy for a busy nurse who’s short on time to use to quickly identify a patient suffering from sepsis. It lives on our Pulse site so nurses know right where to go and print it out.
The checklist starts at triage and follows the patient through the ED. It identifies key vitals to track, symptoms of severe sepsis, steps to take if concern for sepsis exists, and the process for initiating a Code Sepsis. It’s broken down into time frames: what to do within 20 minutes of ED arrival, what to do within 10, 60, and 120 minutes of recognizing sepsis, and how to provide ongoing care to anyone who triggers a Code Sepsis.
All of these guidelines come from the Surviving Sepsis Campaign. There’s research behind it—and since we made the checklist easy to understand and implement, nurses are more willing to embrace it.
Designing education that sticks
To nurses, the checklist feels like support. It serves as a teaching tool, both for new and long-time nurses. The fact that we worked collaboratively with inpatient teams and value engineering to understand our work flow better made the checklist even stronger.
Implementing the checklist wasn’t easy. We started in November 2016 and still work on it every day. It required many, many staff meetings, lots of emails, and it also had to occur in sequence with other improvement projects. How do we design education for the many simultaneous initiatives that are all important? We can’t dump everything on our nurses at once—especially in the ED, where we have 125 nurses, along with more than 100 medics, HUCs, and other support staff.
The checklist as a vehicle for continuous improvement
The checklist has led to success in the ED. Our achievement of perfect care based on the Surviving Sepsis bundle’s guidelines for sepsis management has definitely improved since the implementation. We’ll never be done with this work, especially as we learn new things and stay on the cutting edge of what’s best for the patient. We have to maintain that continuous culture of improvement.
Improvement is a process: we circle back, identify the problem, and then continue to try and implement a solution. We look back at old cases of sepsis and try to find learning gaps to improve on. We’re doing better than last year—but still not as good as we could or should be. We’ll always be working on this project. It’s the kind of work that’s never done.
ED checklist and sepsis protocol led to more patients receiving "perfect care"
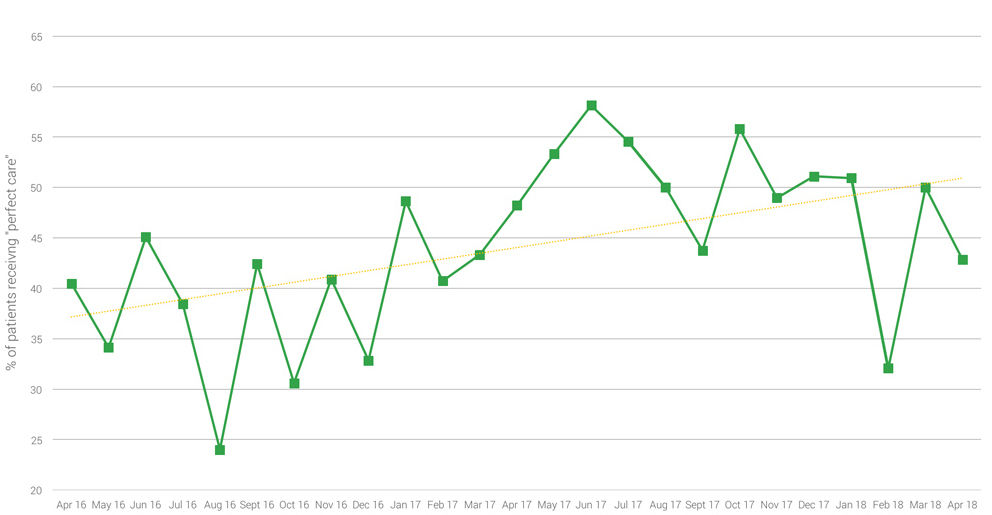
ED’s sepsis checklist has led to an increase in the delivery of perfect care since the improvement project was implemented in November 2016.
View the Value Summary here.
Emilie Johnson
Jamie Troyer
Sometimes the most impactful change comes from simply asking, “Why are we doing things this way?” Pediatric infectious disease professor Adam Hersh explains the impact of practice inertia on antibiotic treatment in pediatric patients, and how questioning the status quo improved outcomes and reduced cost.
Utah’s Chief Medical Quality Officer Bob Pendleton describes a strategic challenge faced by many industries, including health care. We are at risk for prioritizing achievement of metrics over our purpose. He challenges us to think beyond metrics to what patients actually need from us: patient-centered, outcome-focused, affordable care.
Thinking about teams differently did more than improve our inpatient discharge process. It gave everyone a shared vision: every single patient in the right bed, at the right time. Patients now leave the hospital earlier, all while monthly discharges have increased. Tracey Nixon, director of capacity management, shares how they did it.
