What is a Bundled Payment? (Quick refresher)
A “bundle” places all of the care for a certain procedure, or series of procedures, into a single bucket. A bundle. The rationale for contracting for a bundle is threefold:
- Patients benefit from having a team of providers focused on improving care processes, which often result in reduced procedures, supplies, and transition time.
- Payers benefit from having a predetermined price they will pay for care, meaning they know the exact amount they will pay for an episode of care.
- Care providers benefit from knowing the predictable amount they will get paid for patient care, even if the costs associated with that care are less than the agreed-upon bundle amount.
When talking about bundles with both internal and external colleagues some of the first questions are “what bundles do we participate in?” and “how can we establish, or build, a bundle?”
This post will address “how long will it take to get paid?”
556 Days to Payment
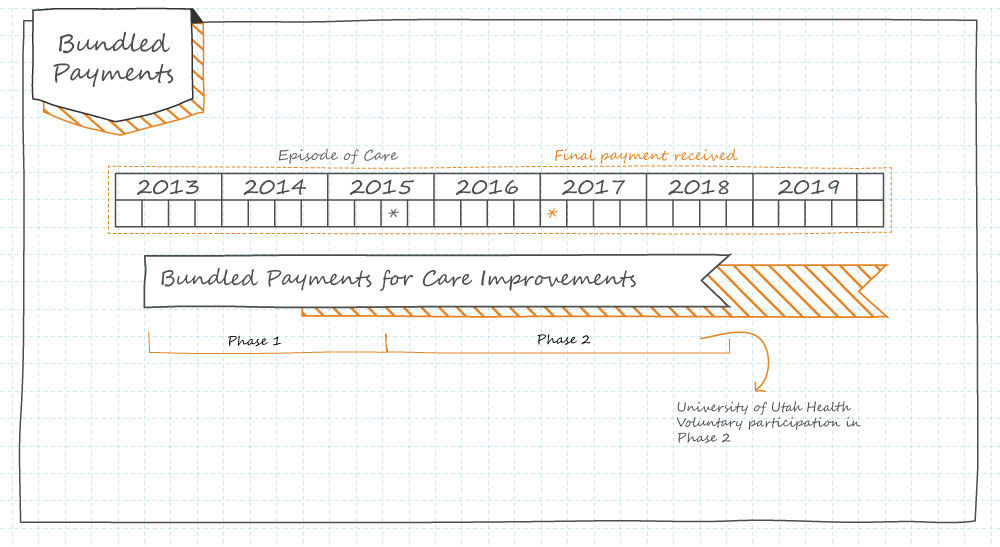
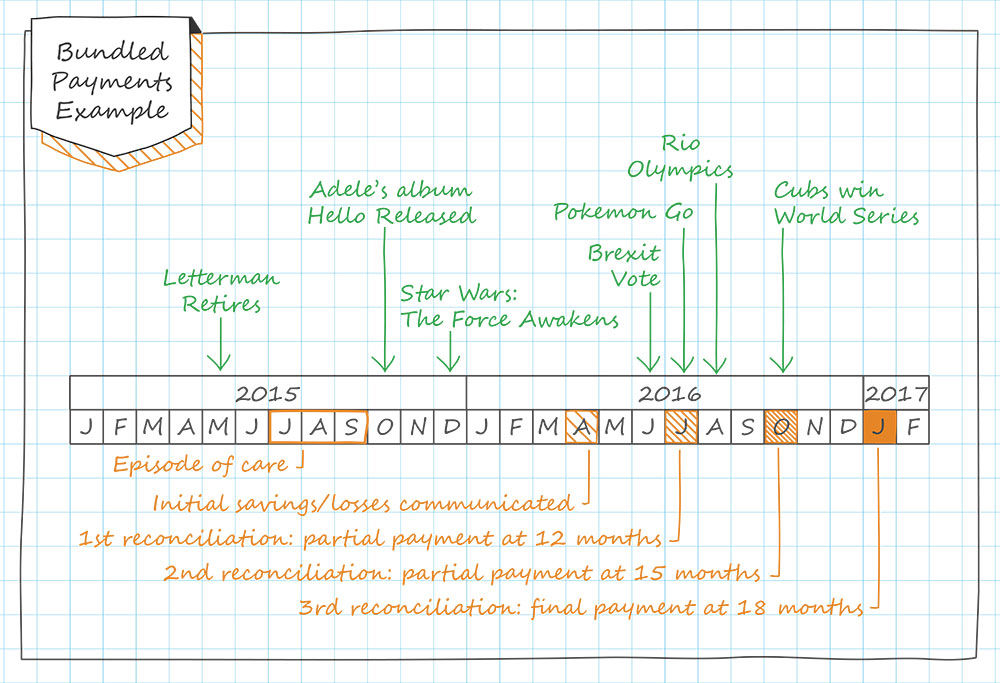
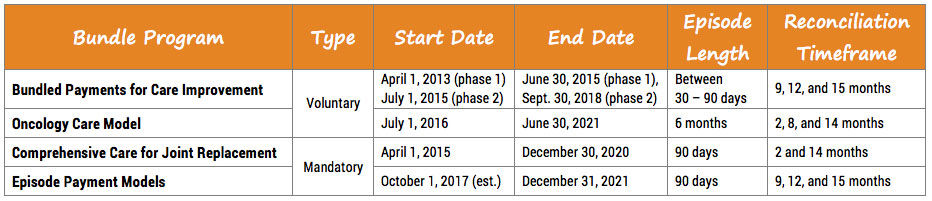
The various timeframes associated with different bundled payment programs are often confusing. Variation abounds - when bundle(s) start/end, when payments are dispersed, how long the bundle(s) last, when financial reconciliation takes place (and what “reconciliation” means), and ultimately when the program sunsets.
The following illustrations are intended to help answer these questions. While it focuses on bundled payment programs created by the Centers for Medicare & Medicaid Services (CMS), these same concepts apply to all bundled payment programs independent of the originating organization.
What 500 days looks like
Bundle timelines
Zac Watne
Patients will ask three things of us over the next decade of health care improvement: help me live my best life, make being a patient easier, and make care affordable. To meet those needs health care must shift—from organizing around a patient’s biology to understanding the patient’s biography.
Sometimes the most impactful change comes from simply asking, “Why are we doing things this way?” Pediatric infectious disease professor Adam Hersh explains the impact of practice inertia on antibiotic treatment in pediatric patients, and how questioning the status quo improved outcomes and reduced cost.
Utah’s Chief Medical Quality Officer Bob Pendleton describes a strategic challenge faced by many industries, including health care. We are at risk for prioritizing achievement of metrics over our purpose. He challenges us to think beyond metrics to what patients actually need from us: patient-centered, outcome-focused, affordable care.