The Big Idea: Be Curious, Don't Blame
How you react to problems is critical in leading and motivating a team. If met with personal blame, people cover up problems, instead of bringing them to light. University Hospital’s Support Services, which includes Environmental Services, has been testing new approaches to problem-solving.
These are their principles:
-
Ninety percent of workplace problems are process problems (not people problems)
-
Uncovering problems won’t always feel good, but it is good
-
Problems are received with curiosity and goodwill (no gotcha!)
-
Making problems visible is part of the job
— Rob Kistler, University of Utah Health’s Senior Director of Support Services
The problem: waiting for a bed
ow fast a room can be prepared for the next patient is critical for a hospital. It means the next patient can start receiving specialized care from the team—nurses, physicians, aides, therapists, and pharmacists. Environmental Services (EVS), University of Utah’s team of custodians, ensures the inpatient stay starts safely by thoroughly cleaning every patient room after a discharge or transfer.
For the last few years, University Hospital has been working to improve efficiency around discharge and admission. We huddle daily, with an interdisciplinary team led by nursing director Spencer Steinbach, to talk through the day’s challenges. After a few years of huddles and consistent improvement, Spencer asked us to think about the room turnaround process.
It's easy to be defensive when another department says you need to improve, but their fresh perspective reaffirmed what we were already seeing. There needed to be a change. We wanted to understand the process and where exactly the delays occurred. We needed data.
Use data to identify your opportunity for improvement
Establish the current state with a baseline analysis
For EVS, room turnaround time starts the moment the patient leaves the room. It shows up in the “dirty” column in the online admission/discharge tracking system, Teletracking, and flags the assigned custodian that a room is ready to clean. Turnaround time includes the time for the custodian to arrive at the room and the time spent cleaning.
We measured our room turn time in Teletracking.
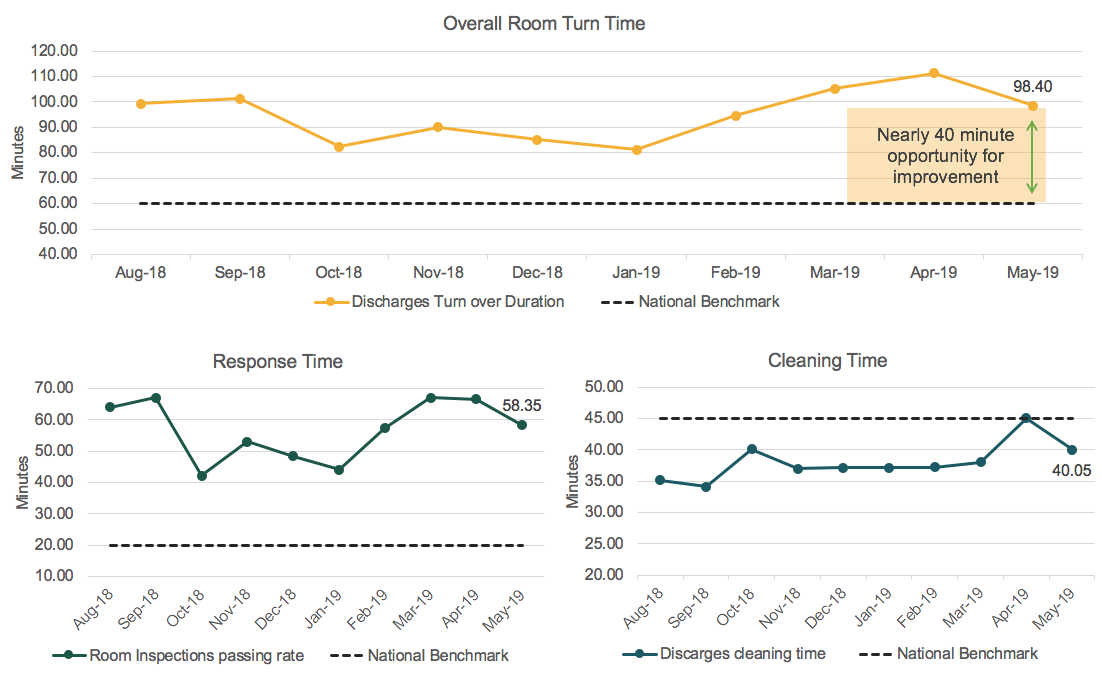
Comparing to national benchmark reveals opportunity
View the baseline analysis process map here.
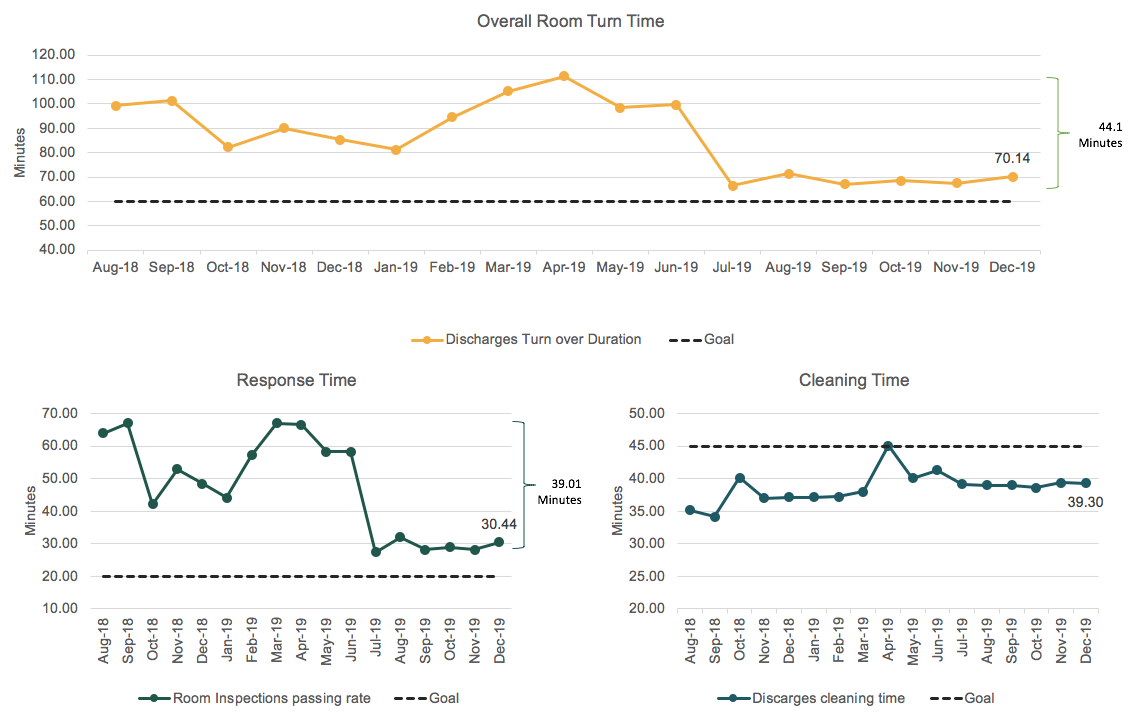
When we started this project, our average turnaround time was nearly 2 hours. It takes 40 minutes to properly clean and sterilize a patient’s room, so the remainder—78 minutes—was spent waiting for a custodian to respond. The national benchmark for overall turnaround time is 60 minutes, fully half of what our turnaround time was. And the national benchmark for response time, the time it takes for a custodian to arrive at the room, was 20 minutes. At 78 minutes, we were way outside of that.
Lastly, we looked at our staffing levels and patient volume by time of day.
Focus your opportunity (keep an eye on culture)
Staffing not aligned to the busiest time of the day
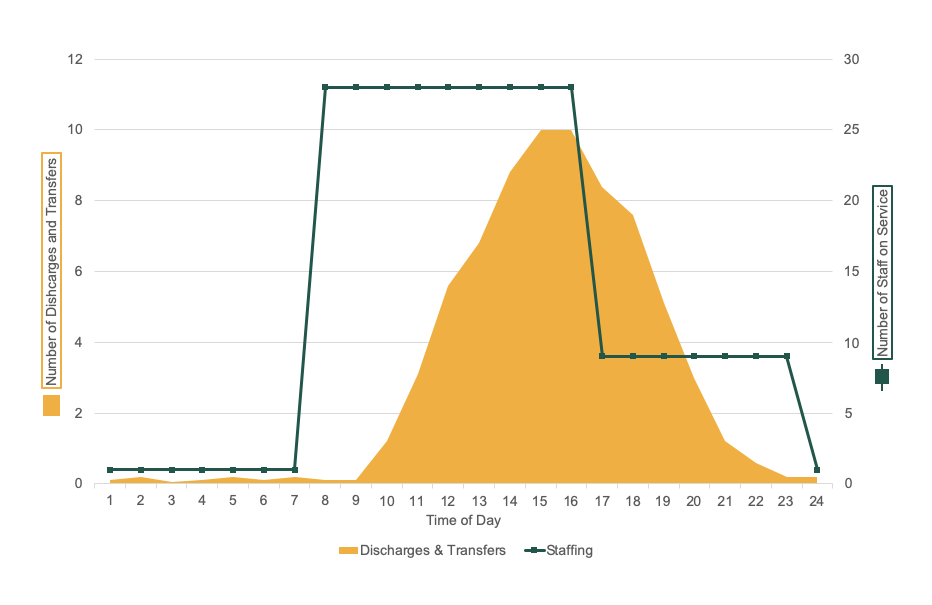
Our unit-organized custodians cleaned occupied patient rooms, and then stopped to clean a discharged room. Early in the day, the response time was usually 5 or 10 minutes. But as the day wore on, more discharges stacked up. At 3 pm, we used to change staffing from a unit-based team to just one team that floated throughout the units. Our analysis revealed that we were changing shifts in the middle of the busiest time for the hospital.
We noticed a lot of blaming and finger-pointing, with teams saying things like “that’s not my job,” or “that team should have done that.” We knew we needed to change both our culture and our processes. Could we develop an organizational structure that supported ownership and resource management?

The solution: culture-driven process improvement
Learn together
We attended a teletracking conference to find other people we could learn from. Amanda Sndyer, Support Services Project Administrator and Dane Falkner, Sr. Value Engineer, helped us think through the problem and possible solutions.
Address ownership
We had an ownership problem in EVS. Because our teams switched over at 3 pm, there was a feeling that whatever happened after 3 pm “isn’t my problem, it's your problem.” We needed to find one team to own discharges across the day.
We found it was also challenging for our custodians who cleaned rooms occupied by patients. When we were busy and had a list of discharged rooms to clean, custodians felt like they had to delay lunch in order to clean a room. To think about removing that weight on our custodians was a big deal for them.
We decided to go from a “generalist” to “specialist” model, establishing a single team that would own discharges.
Meet the demands of the bottleneck through load leveling
Our baseline analysis revealed a bottleneck: dirty patient rooms stacking up after 3 pm. We wondered if we could change staffing to address the bottleneck. We wanted to be very careful about adding any FTEs, so we looked at the right time for our shifts to start. Originally we had three 8-hour shifts beginning at 7 am, 3 pm, and 11 pm, but if one group got behind, employees on the next shift were constantly playing catch-up. Shortly after 3pm, the emergency department starts to get busy, which compounded delays.
We decided to start shifts at 7 am, 12 pm, and 3 pm, stepping up our staffing volume during the busiest parts of the day and scaling back during less busy times. This is called load leveling, and it refers to balancing the different parts of the process to reduce delays.
Tackle the hard topics: employee schedules
As we started to put together the new discharge team’s schedule, we worried about adding more employees. We looked at all of the daytime teams and wondered if we had the right number of people—could some people float to this new team? We soon realized that we had to address how each team scheduled. Each supervisor had the autonomy to schedule their own teams. While it gave a sense of ownership, it reduced the effectiveness of the overall EVS team. We decided to have one person do central scheduling for everyone so we could cover every team appropriately, every day.
"It was a hard change. Anytime you schedule for 250 people, you’re not going to make them all happy."
It was a hard change. Anytime you schedule for 250 people, you’re not going to make them all happy. Some were worried that the new team would take resources from existing teams. Some senior employees felt they were losing priority scheduling, while junior employees felt better about not having to always work the less-than-prime shifts. We kept emphasizing that the change would not only accommodate patient demand, it would also support the custodian.
Listen to the team
We introduced the changes with a big party and then asked for the team’s input on equipment and supplies. We asked about the other delays they experienced. That’s when we learned about the time-consuming phone calls.
In every discharged room, the custodian had to place a 30-60 second phone call to track the room’s status so the admitting team could then signal the transport team that a room was available. The time spent on the calls added up quickly. We introduced iPads that would provide the same information about room turnaround progress, but with a simple click, saving two to three hours of team time every day.
We also created a centralized stock of equipment that was necessary to clean each room so people wouldn’t have to search for missing supplies, further reducing turnaround times and eliminating waste.
Implementation: go-live and then reassess (PDSA)
On October 3, 2018, we launched the first of our new processes and started tracking our progress on the Teletracking monitor (we phased our implementation). The first few hours seemed great because there were no discharges. By noon, we started seeing that our changes hadn’t worked in the way we planned. After two days of watching, we could see we weren’t going to hit our goal of a 60-minute turnaround.
Initially, despite the streamlined workflows, our numbers got worse and morale was low. We knew we couldn’t go back to the old way, though, so we reexamined the data to see what we were missing. We discovered that our initial data on discharge volumes didn’t include the women & children’s area, and that additional volume was leaving us perpetually short-staffed.
While our initial goal had been to keep FTE numbers flat, we knew that we could never meet the demand with current staffing levels. We requested eight additional FTEs and finally saw progress within a few months.
The outcome: what we learned
View the process map after improvement (current state).
It was important for us to be open-minded, patient, and focus on where we were going by looking at the data. Patience was especially important—without it, we wouldn’t have stuck with our goal after encountering the initial bumps.
This change required a lot of difficult conversations. With any big change, it’s important to cultivate a culture of improvement with support from top-level leaders who are engaged and listen to the entire workforce.
EVS is a very diverse team, representing over 20 countries and various levels of education. Instead of avoiding the conversation, we involved them in the conversation. Empowering people to be heard and providing their insight brings out the best ideas. As scary as it is to engage people who may be opposed to what you want to do, their opinion helps avoid future problems.
We're still learning and continuously improving, while monitoring our progress.
Results: 45 minute improvement
James Mwizerwa
Cooper Riley
Feedback is a gift—even when it doesn’t feel like it. Senior Director of Care Navigation Stacy Silwany teams up with Organizational Development’s Michael Danielson to share how Care Navigation uses WellCheck survey data to learn from and engage employees in making the workplace better.
Why do some organizations thrive during a crisis while others flounder? Iona Thraen, director of patient safety, joined forces with her ARUP Laboratory colleagues to learn how the world-renowned national reference lab adapted to the pandemic. Leaders created a culture of safety by putting innovation, learning, and patient-centered care at the heart of all their efforts.
U of U Health recently received the LGBTQ Health Care Equality Top Performer designation from the Human Rights Campaign Foundation—but this achievement didn’t happen overnight. Plastic surgeon and Transgender Health Program Director Cori Agarwal, and Program Coordinator Ariel Malan, share the grit, determination and patient collaboration that transformed our health care system.
