providers, the responsibility is on us to manage patients’ expectations. I try to set consistent expectations with my patients; I think patients will be respectful of your time if you are respectful of their time. Patients are much more sophisticated than we give them credit for. They have expectations for communication between appointments. They expect to quickly receive their results. I had to learn how to incorporate the notion that away-patient work is just as important as patient-in-the-building work.
MyChart helps manage patient expectations, but have a process
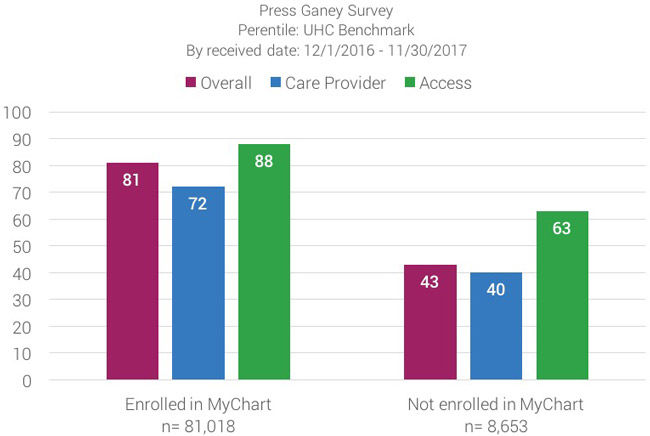
I leverage MyChart, even though it’s a cruel mistress. Patients love technology, whether physicians like it or not. Satisfaction scores show that 81% of patients with MyChart accounts have an overall better experience versus 43% of patients who don’t have a MyChart account. That reduces the uncertainty that comes from waiting for appointments, results, and communication.
Want to double your patient’s satisfaction? Have a MyChart process.
Gone are the days when you could say, “You will have your results—and your lives—back in a week or two.” Why let those results just sit there and fester in the fermenting cave that is your in-basket when letting patients see them reduces their anxiety? Now, patients can have their lives back tomorrow—sometimes today.
At the same time, you must balance the use of electronic medical records with your own wellness. EMR is one of the single biggest contributors to provider burnout. Yes, it makes my patients happy to receive their results in a day or two, but I have to manage those results well or my work-life balance suffers.
I never dreamed when I went into health care that I could work from home. I chose a job where I knowingly would never work from home. But I work from home all the time now. I can have dinner with my kids, then work an hour at night—what we call “pajama time”—to finish what I left.
It’s an ongoing balancing act. I’m not tied to the office anymore. With my phone, I can answer refill requests while waiting in line at the grocery store. Soon, with my Apple Watch, I’ll be notified when a patient receives abnormal results. This rapid response to my patients increases their feeling of coordination and patient-centered care. But is it more “pajama time”? MyChart helps manage patient expectations, but use it wisely.
What Is "Pajama Time"?
Defined as administrative work completed after hours or at home, a recent study found family doctors spend an average of 86 minutes of pajama time each night.
Clinic flow can improve teamwork
Your team is important—they can help reduce “pajama time.” It’s not so much you as who’s framing you. With help from Senior Value Engineer Matt Sanford, my office at Redstone Health Center has recently introduced new clinic flow concepts. My medical assistant Allison Kubik has taken charge so we run on schedule as a team. Our workflow is as follows:
- Allison rooms the patient and writes the HPI [history of the present illness].
- She informs me of the whole story. By the time I’m in the room, I ask a few additional questions.
- While I’m in the room, Allison goes through my in-basket and writes down the top three things I must do once I’m done with the current patient and before I see the next patient: call this patient to manage his or her anger, help this patient understand a scary test result, celebrate with this patient whose result came back clean.
Allison controls my flow, which helps me stay focused. She has to know that she can interrupt me — and that I’m not going to yell at her. I had to agree to be bossed around. It all comes back to being respectful of a patient’s time.
Better teamwork can reduce patient uncertainty
Empowering my team helps me deliver more responsive care. Because Allison is engaged in my practice, I can tell a patient, “Call and ask for Allison.” She’s there every day—and on the days I’m not there, she looks at my messages and can respond to patients. That communicates, “Work at the top of your license.”
If you’re a medical assistant and it’s within your license to answer a patient’s question, then you should be empowered to do it. Empowered MAs allow me to focus on the tasks that only I can perform. Only I have the ability to sign a doctor’s note or order a refill of a prescription.
More time helps me to run on schedule. Patients gravitate to me because of my respect for their time. My patients know they will get into the room on time, they will be seen, and they will get out. They’re not going to be there all day. I’m not going to waste their time, and it shows I respect them.
Melissa Briley
Improvement isn’t just for one area of academic medicine. The right improvement can mean improved patient and trainee experience, reduced cost and a more engaged staff. Nurse Manager Bernice Tenort, physician Brett Einerson, and an interdisciplinary team ended up solving many challenges by tackling a long-standing problem: wait time in labor and delivery.
When dermatologist Dr. Stephanie Klein proposed a clinic for urgent skin care needs, she thought it would be easy. Reserve the clinic rooms, schedule the appointments—done! She quickly found out that moving from idea to reality would require leadership skills that she hadn’t been taught in medical training and ten years of practice. Accelerate’s Mari Ransco found out how Klein transformed from busy clinician to leader.
Trust. That’s what we want. We want to earn and keep the trust of every patient. We want them to trust that we provide the best possible medical care. But more than that, we want them to trust that we will respond to their needs, coordinate our efforts, and provide them with available options. We want them to trust that we will answer our phones, explain their treatment, and value their time. The exceptional patient experience is an enterprise-wide system designed to deliver a singular output: trust. And, this enterprise-wide system is built on trusting our providers and our teams.
