epression is serious. Nationally, self-reported lifetime prevalence rates average 17.6%; here in Utah, that number is 20.8%, ranking us among the top 10 in the US. As part of its Healthy People 2020 initiative, the United States Preventative Services Task Force recently recommended that all patients 12 and older receive depression screening. That’s important: research conducted by Luoma and colleagues found that 45% of suicide victims had contact with their primary care provider in the month before their death.
As quality improvement specialists, we work with all of U of U Health’s Community Clinics and the Department of Family and Preventative Medicine’s primary care clinics. Working with data analyst Jordan Ballam, we saw that fewer than half of our patients were screened for depression.
11 clinics, 1 goal
We asked 11 community clinics—Centerville, Westridge, Farmington, Redwood, Redstone, Madsen, Parkway, Sugar House, Stansbury, South Jordan, and Greenwood—to work on the same project at the same time. Our team spends significant time embedded in all of these clinics, so we were able to bring interdisciplinary teams together to discover how we could improve.
We started with baseline analysis. The percentage of patients 12 and older who saw their provider and completed some form of screening (PHQ-2, PHQ-9, PHQ-A for adolescents, Geriatric Depression Scale screening, or mEval PROMIS depression screening) in the last year was low—40.75%. Most had already been identified as having depression, so we knew we weren’t catching new patients.
Consensus-driven improvement
Each clinic was asked to identify methods that could work in their local environment—and each one independently came up with a version of the same intervention.
First, we enhanced our pre-visit planning and created visual reminders in Epic to help providers prioritize the patients’ needs. We provided extra education to MAs and other clinicians, helping them identify the right screening tool for the right patient, the right way to administer the tool, and what to do with the results.
During our analysis, we found that patients needed more opportunities to complete the depression screening. We added new tools, such as mEval sent to patients prior to their appointment, paper forms, computer forms in the exam room, and non-English tools.
When patients reported depression, hand-offs to behavioral health resources such as on-site social workers, crisis assessments, therapy sessions, and referral to outside resources,= occurred immediately.
Result: More people getting the help they need
Prior to the project kickoff in October 2017, depression screening rates across all 11 community clinics was 40.75%. By February 2018, that screening rate had increased to 54.5%. Every single clinic made some sort of improvement, however.
Throughout this project, we found quite a few examples of patients who were suffering from depression (and perhaps had been for some time) but hadn’t felt comfortable discussing it with their provider. Now, more patients can get the help they need.
At the end of the day, the success of this project boils down to the fact that we were willing and able to spend time getting to know people in the community clinics. With every quality improvement project, we observe, interview, understand, and respect each clinic’s local culture. Now, depression screening is part of the Healthy Planet dashboard, and any provider can access their data at any time.
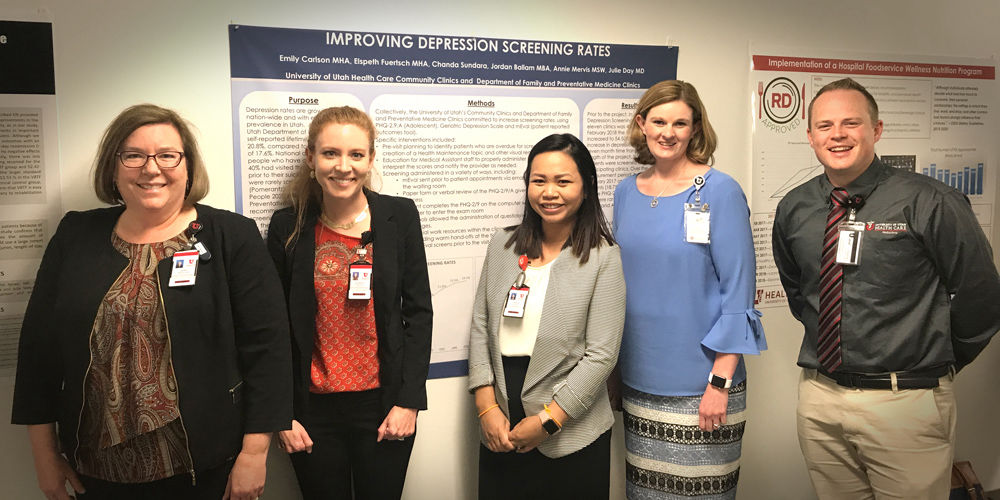
Evidence-based practice "Best of the Posters" honoree
Of the 46 projects submitted for consideration at the April 2018 Evidence Based Practice Poster Fair, this project was one of three selected for presentation at the “Best of the Posters Session.” We applaud these efforts to share and spread best practices in delivering high-value health care within our community and beyond. Learn more here.
Emily Carlson
Elly Fuertsch
Chanda Sundara
The hard work of improving value includes leading and engaging a team. Two improvers, Emily Carlson and Dr. Lauren Wood, share how they kept their teams engaged throughout a long (and sometimes inconclusive) improvement process.
Thinking about teams differently did more than improve our inpatient discharge process. It gave everyone a shared vision: every single patient in the right bed, at the right time. Patients now leave the hospital earlier, all while monthly discharges have increased. Tracey Nixon, director of capacity management, shares how they did it.
Biometric identification is a national best practice — but adapting that to a local environment isn’t easy. Although it’s rare, confusing an identity can have scary consequences (like getting a prescription for a drug you’re allergic to.) So Doug Ostler and his team worked to implement palm scanners and make patients feel safer.