The Challenge
The Value Equation of Nursing Shift Report
Effective handoff between nurses is one of the most important processes to reduce safety errors and promote patient-centeredness. The challenge is to exchange this information in the most efficient manner possible, eliminating the waste of wait.
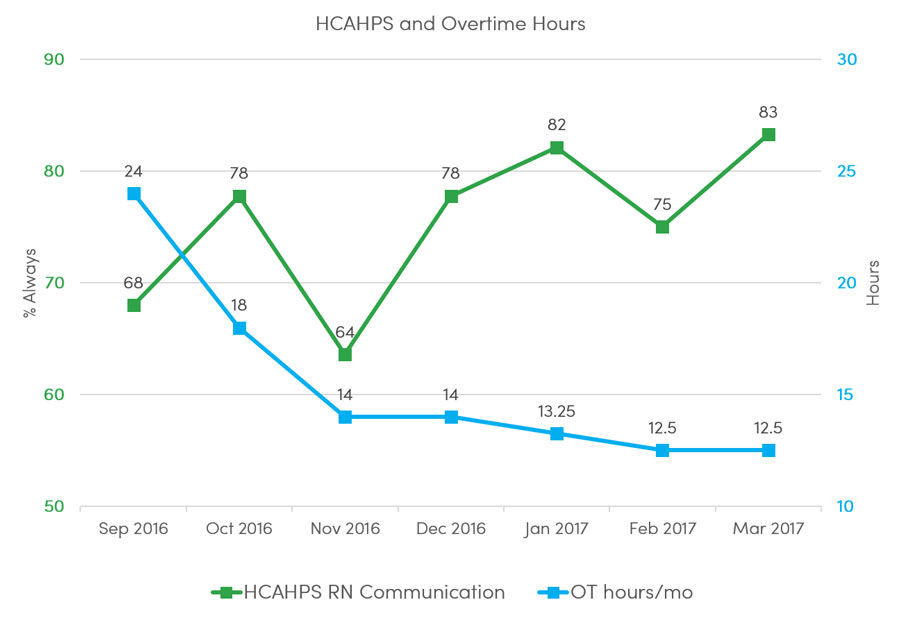
Utah’s value equation is defined by the patient and it is Value=Quality+Service/Cost. This case study demonstrates that reducing cost (unnecessary overtime) does not negatively impact safety or service, as represented by D’Ausilio’s balance measure (HCAHPS).
urse shift report has three parts: an all-hands safety briefing, receiving patient assignments from the charge nurse, and finally bedside report with the off-going and oncoming nurse in the patient’s room. It’s one of the oldest processes in the hospital and stubbornly tagging along with it is one of the oldest problems: It often runs long, cutting into off-going nurses’ personal time, and hitting managers’ budgets with overtime cost.
One popular way to address the financial and work-life balance challenge is to encourage (and later admonish) nurses to “pay attention,” and, “be efficient.” At best these traditional interventions achieve short-term success. The value improvement methodology will likely feel counterintuitive if shift change woes are thought of and treated as a people problem. If recognized as a process problem, the methodology makes sense, calling for an examination of the “it’s always been done this way” problem (in this case, shift change), to pinpoint delays and identify and prioritize their causes. The real challenge is to persuade time-starved leaders to invest the effort to better understand the problem to reveal new, more effective solutions.
Background
Nurse Jamie D’Ausilio took the helm of University of Utah Health’s inpatient medical rehabilitation (IMR) unit in 2015. IMR is a 38 bed unit with 45 nurses and 45 health care assistants (HCAs), and the team cares for patients recovering from an acute episode. D’Ausilio became the nurse manager just as design for a new rehab hospital started. Despite her current and impending workload, D’Ausilio decided to take U of U Health’s lean six sigma green belt, equivalent to an upper level college course. She and her value engineer coach Mitch Cannon discussed the time commitment and project the course required. Was it really the time to take on this educational challenge?
Yes, it was the perfect time, thought D’Ausilio. She believed that building her value improvement skills would actually help her save time. D’Ausilio had read process improvement books on her own and the concepts made sense. If she could expand her skill set, she could help her teams find better solutions to daily problems—solutions that would keep working after she moved onto the next issue. But reading about the skills was not enough. D’Ausilio wanted to attend a structured class to help her apply the skills properly. The lean six sigma green belt class required a project, and D’Ausilio soon discovered an everyday, long-standing problem to explore: unnecessary nurse overtime. She examined her payroll data and found many late punch outs. It wasn’t one particular nurse or shift – it was pervasive. Minutes were adding up. D’Ausilio applied the value improvement methodology she was learning in class.
1. Project Definition
In the first phase, called project definition, D’Ausilio thought about why this project mattered and who would help her reduce nurse overtime. This phase includes identification of the team, vision, and scope. Because the value improvement methodology emphasizes the importance of involving those who do the actual work in the investigation and design, D’Ausilio included a small group of charge nurses, floor nurses, and her clinical nurse coordinator, Nicole Lynch, on her team. Together they crystallized their vision for the project: why this is important work, how it will benefit nurses and patients, and so on.
The problem statement: D’Ausilio wrote a SM-RT (specific, measurable, reliable, time-bound) problem statement. She found that IMR accrued an average of 30 hours of nurse and HCA overtime in fiscal year 2016. Sometimes spikes occurred—in July 2016, IMR accumulated 57 overtime hours despite the unit’s full staff.
SMART goals: D’Ausilio wrote a companion SMART (specific, measureable, attainable, relevant, time-bound) goal. Specifically, D’Ausilio established an outcome measure: to reduce costs by reducing monthly overtime from 30 hours to 15 hours in six months. To ensure whatever improvement implemented did not have undesired side effects (such as reducing time spent with patients), D’Ausilio chose a balance measure. Nurse communication, as reported by the HCAHPS survey.
2-3. Baseline Analysis and Investigation
Why were nurses and HCAs leaving late? D’Ausilio’s analysis included the payroll data and a current state process map. She found that indeed, leaving late was not isolated to a particular event or person. There was something about the process of shift change.
Going to the gemba: D’Ausilio and her team visited the workplace as an observer, not as a boss or an experienced nurse. They watched the shift change process in action from start to finish, called going to the gemba. They were surprised by the length of safety briefing. The team watched some nurses complete bedside report right on time and others take an extra 10-15 minutes.
Fishbone diagram: D’Ausilio facilitated her team in a categorical brainstorming session using a tool called a fishbone diagram (aka, cause and effect diagram). D’Ausilio’s goal was not to crowd source solutions, but to really understand the causes of the problem.
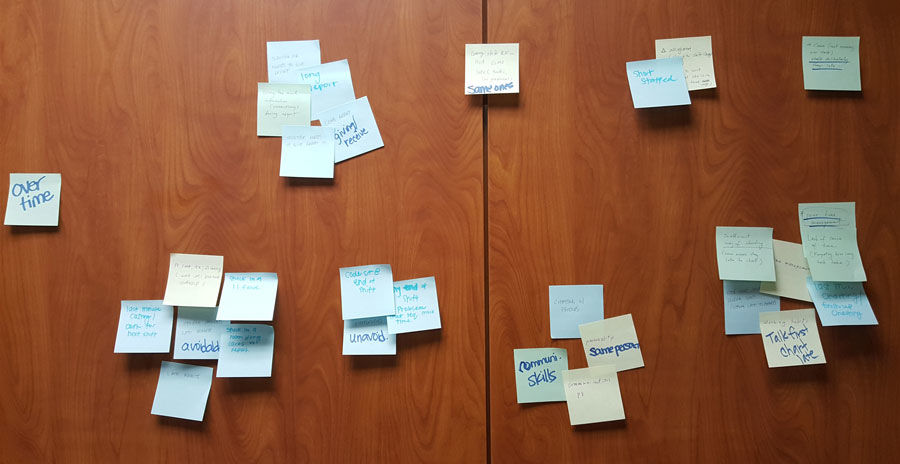
The team used post-its to organize the causes and effects of overtime
The team's fishbone diagram organized the causes and effects by affinity
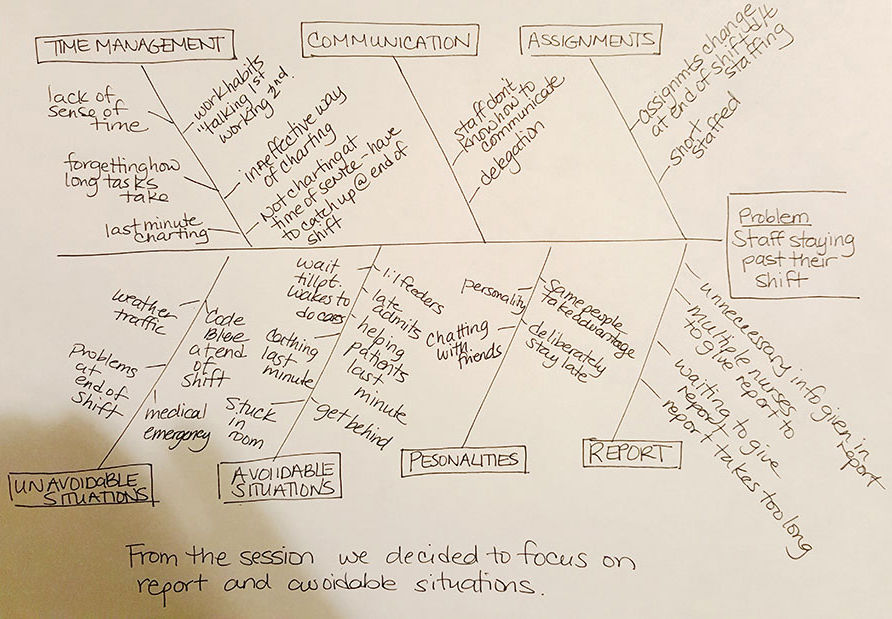
The fishbone diagram revealed a compounding problem: the number of nurses giving and receiving shift report. Typically, each nurse is assigned four patients. An oncoming nurse might have to coordinate bedside report with four off-going nurses. Meanwhile, each of those nurses could be waiting for three additional off-going nurses. These multiple pairings lead to searching the unit for the next bedside report and periods of delay as nurses wait for bedside reports to end.
The team carefully reviewed their findings from the analysis and investigation and concluded safety briefing and waiting for multiple nurses to give or receive bedside report were their biggest opportunities. One particularly significant finding: if off-going nurses gave report to three or fewer nurses, they could likely end shift on time. Now, what to do with all this new information?
4. Improvement Design
Reducing the time requirement for safety briefing: Safety briefing shares important safety risks from the past shift with the entire nursing team. The original process involved the off-going charge nurses preparing a summary of each patient on the unit and then reading the summary aloud to an assembly of oncoming nurses and HCAs. This process required everyone to be in the same place at the same time. The first to arrive waited on everyone else, and everyone waited on the last person to arrive.
D’Ausilio developed a future state process map.
In a classic example of visual workplace management, D’Ausilio proposed that the information wait rather than the people. The charge nurse now posts the written briefing in a central location and each oncoming nurse initials that they read the brief. The new process reduces waste in two ways: people can read faster than they can listen, and posting the brief eliminates all waiting. As a quality check, D’Ausilio implemented spot checks with nurses to be sure they had the needed information.
Reducing wait time for off-going and oncoming nurse pairs: The second intervention would be much more complex. In making nurse assignments, IMR charge nurses balanced the number of patients with nine other individual patient factors, including complexity and acuity. Before her lean six sigma green belt class, D’Ausilio might have solved this through charge nurse education with a promise to “do better,” but clinical nurse coordinator Nicole Lynch took on the challenge to do better than just “do better.”
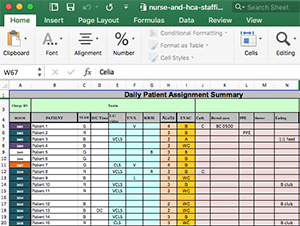
Originally, charge nurses kept track of the assignments manually. In a demonstration of process benchmarking, Lynch brought the problem to a family dinner. An accountant at the dinner (her father) explained how he had solved similar problems in Excel. Together they expanded on his idea producing a dynamic visual management tool to balance all of the criteria for patient assignments.
5-6. Implementation and Monitoring
D’Ausilio piloted both interventions across the unit starting in September 2016. The project was done, with only monitoring left. The results were immediate and impressive. Avoidable overtime decreased by half and projected annualized saving is $12,000 while HCAHPS scores improved. Importantly, nurses are leaving for home on time.
Overtime hours have steadily decreased while RN communication improved
View the Value Summary
IMRU Lean Six Sigma Project: Decreasing Cost of Overtime. Cannon M, D'Ausilio, Hernandez J, Lynch N, Trujillo C. University of Utah Value Summary. 24 Aug 2016.
XReflection
Solving the age-old problems of health care doesn’t require more solutions. It requires better understanding of problems. D’Ausilio moved past the traditional management strategy of asking for promises of vigilance with the implied threat of sanction. Instead, she took on process change to effect a permanent improvement for her staff and her budget (and earned a lean six sigma green belt).
Chrissy Daniels
Mari Ransco
Steve Johnson
Nicole Lynch
Jamie D'Ausiolio
Your gut tells you a process could be better than it is—how do you back that feeling up with hard data? Senior value engineer Luca Boi shows how undertaking a baseline analysis can jumpstart your improvement project.
Safety as a value requires a cultural shift, not just getting people to talk about patient safety but to know how it impacts everything we do. U of U Health’s Director of Patient Safety Iona Thraen draws from the personal to highlight a system-based approach for moving from reactive to proactive patient safety.
The practice of medicine is recognized as a high-risk, error-prone environment. Anesthesiologist Candice Morrissey and internist and hospitalist Peter Yarbrough help us understand the importance of building a supportive, no-blame culture of safety.