March 16, our world of providing patient care changed dramatically. Aside from the significant changes to treat patients with COVID-19, patient care in many of our clinics came to a halt literally overnight. While we’re keeping patients out of harm’s way by avoiding exposure to the the coronavirus, delaying care for an extended period of time has other consequences.
Within three days our department postponed more than three weeks' worth of visits - 1,000 patients. We realized that waiting this out would only exacerbate the long delay patients already have to see us when we resume in-person visits. We also have no idea exactly how long the current restrictions will continue, or what the “new normal” will look like, so we needed to create a model that prepares us for uncertainty ahead.
Since conditions in neurology and other specialties do not pause, even in a global pandemic, now is the time to start implementing real workflows for available virtual health technologies.
Guiding Principles of Virtual Visits
Virtual visits are not the same as in-person visits, but there are some things that we wanted to carry over from our traditional practice. These guiding principles helped us ensure that every patient receives the care they expect and deserve, and our teams can still work efficiently.
- Video visits, like in-person visits, can and should create a true personal connection.
- Virtual appointments will not be the same as in-person visits, but can still be valuable.
- We will not assume that certain types of visits or certain people cannot participate in a virtual appointment.
- Workflows should be comprehensive and use familiar protocols.
- Workflows should work across multiple platforms (MyChart, InTouch, Zoom).
- Start small with a pilot group and adjust as needed.
- Start thinking now about how to design processes that will endure after this crisis.
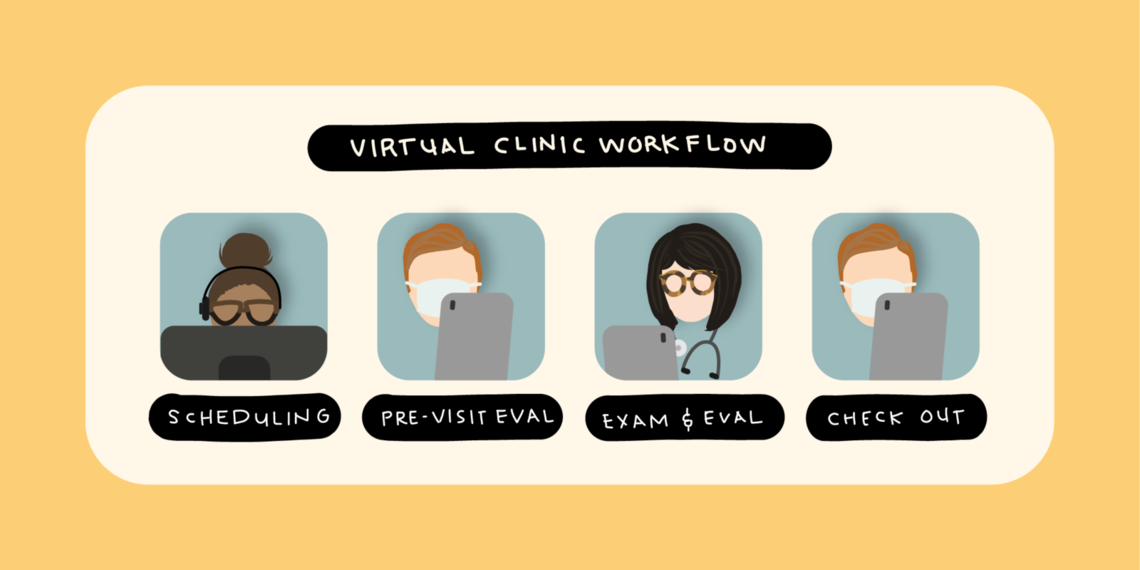
Transforming to a Virtual Clinic
We had to move quickly to start seeing our patients virtually and slow the tide of postponed appointments, but we also knew that this was not the time to radically alter the workflows that our providers and staff understand. We designed a virtual workflow that mirrors traditional clinic visits and tested it out with a small pilot group. After some adjustments, we’re rolling this out to as many visits as possible.
1. Scheduling (at least 3 days in advance)
Schedulers reach out to patients and:
- Confirm which platform will work best
- Send an appointment reminder with links to the video visit
- Create a simple electronic invitation for the provider that includes links
- Offer a chance for both the patient and the provider to test the technology in advance (avoiding delays from technical difficulties)
2. Pre-visit Evaluation (1-2 days in advance)
In a traditional clinic workflow, medical assistants (MAs) conduct a pre-visit evaluation while rooming the patient. Rather than asking providers to do these evaluations and try to use unfamiliar tools they may have never used within the EHR, our MAs still conduct these pre-visit evaluations over the phone one or two days before the visit.
The MA works to:
- Review clinical information
- Ensure the patient’s records are available and correct
- Review medications and answer patient questions
- Document everything in the EHR
3. Exam and Evaluation
The provider starts the visit with the scheduling link. When the patient joins, the provider can begin the evaluation and exam. Since the provider is not in the room with the patient, the provider may need help with parts of the exam, and it’s okay to ask caregivers or family members to participate by holding the camera or helping the patient walk.
There are also some additional post-exam administrative tasks that were not part of our traditional workflow, but are necessary to move the patient’s information digitally to the next step.
After the exam, we:
- Document your note
- Put in any orders for follow-up care
- Send the information electronically to the scheduler and the MA for follow-up
4. Checkout
The checkout process for virtual workflows takes places in the days following the visit.
- The MA or RN is notified electronically
- They contact the patient to schedule any necessary care, such as imaging, tests, or appointments
- If a patient requires urgent follow-up care, we do not assume people will see the electronic communications. We make a phone call if it’s urgent (we shared cell phone numbers among staff and clinicians to facilitate communication).
Tips to Make Virtual Visits Easier
For patients, providers, and clinical staff, the move to virtual visits may have a few bumps along the way. Here are a few things that make it easier as you’re getting started.
Set Up
Many virtual visits right now will take place from your home.
- Set up your computer in a place with a simple background–no moving items, and plain or virtual backgrounds work best (there are virtual background or “background blur” features on video platforms).
- To protect patient privacy, find somewhere you can conduct exams away from family members who are home with you right now.
- Use a bright light in front of you, with limited or no backlighting (including windows).
- For optimal sound, use a headset. It’s difficult to purchase a headset right now, so if you don’t have one and you experience feedback, turn the speaker volume down.
Patient Considerations
Some of your patients may be participating in video visits for the first time as well, so you can help them create a better experience with these tips:
- If they are using a handheld device, such as a smartphone or tablet, place the device on a solid surface to keep the camera steady.
- Try to be in a well-lit room with little or no backlighting.
- Family members or caregivers can assist with the exam as needed.
Video Conduct
Just like an in-person visit, you need to be present with the patient at all times during a virtual visit. It can be more difficult with a virtual visit if you find yourself distracted by technology or surroundings, so:
- Look directly at the camera when speaking with your patient.
- If you need to multi-task, for example, to take notes or find information, explain what you are doing and why you are multi-tasking.
- When you are on video, you can’t use body language so make sure you address people by name to ask questions.
Making the change to virtual visits is not easy, but this current crisis has provided a valuable opportunity to transition to a format that will be an increasingly important part of clinical care moving forward. Now is the time to create efficient and effective workflows and templates that you can build on as you move your practice into the future.
View the complete step-by-step Clinical Update video
View the slide presentation only
Susan Baggaley
Vivek Reddy
Why do some organizations thrive during a crisis while others flounder? Iona Thraen, director of patient safety, joined forces with her ARUP Laboratory colleagues to learn how the world-renowned national reference lab adapted to the pandemic. Leaders created a culture of safety by putting innovation, learning, and patient-centered care at the heart of all their efforts.
Director Lora Stratton details how Utah’s Cardiovascular Center leveraged team creativity and rapid problem solving to make—and sustain—the shift to virtual care. Cardiologist Anu Abraham shares what it looks like in practice.
The Zero Suicide initiative has been shown to significantly reduce suicides—and working toward zero suicides is our mission. Rachael Jasperson, Zero Suicide program manager, shares the framework for how we strive for this aspirational goal.