a physical therapist, I get to fulfill my passion for helping people recover from injuries and work with patients who are battling chronic pain everyday.
Lately, life stressors have made it harder for patients to focus on their physical therapy. Parents, especially, are prioritizing everyone and everything, except themselves. Covid-related pressures like school changes are diverting time and energy away from therapy.
As stress has escalated significantly this past year, many patients have missed appointments, cut back on their exercises, and experienced higher levels of pain. I’ve had many heart-to-hearts with clients who are struggling to give themselves a break. They feel like they’re letting me down.
What has been helpful is supporting patients to alleviate their stress, and in doing this, patients are then able to recommit to their recovery. I have found the following mindful techniques to be especially effective.
Manifestation of physical stress
The link between the brain and the body is undeniable, especially in regard to chronic pain. Physical pain can manifest itself in many ways. One study showed that people with higher depression and anxiety scores also demonstrated worse grip strength, decreased lung capacity, and more inflammatory responses. These are all indicators of pain and how the body reacts to it.
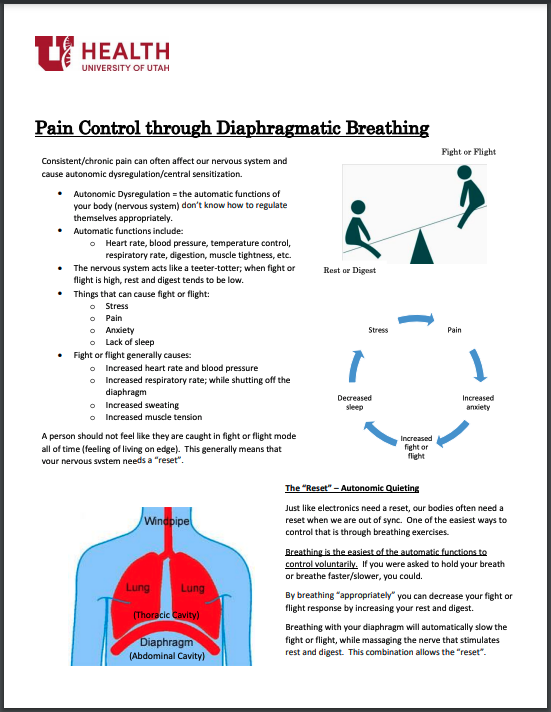
Chronic pain affects our nervous system and can cause autonomic dysregulation or central sensitization. When the nervous system doesn’t know how to respond to different stimuli, the body’s automatic functions can’t regulate themselves.
Some of these automatic functions include:
-
Heart rate
-
Blood pressure
-
Temperature control
-
Respiratory rate
-
Digestion
-
Muscle tightness
Our nervous system acts like a teeter-totter—it seeks equilibrium by balancing our fight-or-flight and rest-and-digest impulses. People with higher pain levels often experience heightened fight-or-flight responses, which throws the nervous system off-balance. Things like stress, pain, and lack of sleep trigger these responses. When we’re stuck in fight-or-flight mode, our automatic functions stop working properly.
Three steps to lower stress
Like our electronics, sometimes our nervous system just needs a reset. Here are three ways to combat physical stress:
1. Breathing
Diaphragmatic breathing
In fight-or-flight mode, our diaphragm, the primary breathing muscle, shuts off. We often try to compensate with our neck and shoulder muscles, which can cause scalene and upper trap tightness. By turning our diaphragmatic breathing back on, we can actually send a “reboot” signal to the brain to help reduce fight-or-flight responses and increase that rest-and-digest action.
Contrary to popular belief, diaphragmatic breathing isn’t belly breathing. The diaphragm is actually a big dome in the ribcage. It’s like a balloon: when we breathe, we press the top of the balloon together, and it pushes the edges out. Our lower ribs expand to accommodate the balloon, or diaphragm.
You can practice diaphragmatic breathing by placing your hands on your lower ribs. Try to breathe the air right into your hands.
Meditation
While diaphragmatic breathing can help alleviate pain, we can also reduce fight-or-flight responses by quieting our brain. Meditation helps with this. However, meditation can also be somewhat challenging, when encountering pain or stress. Quieting the mind takes practice, but one of the easiest ways is to think of one simple thing, like a color, candle flame, or piano. When your thoughts start to wander, refocus your mind on that singular object.
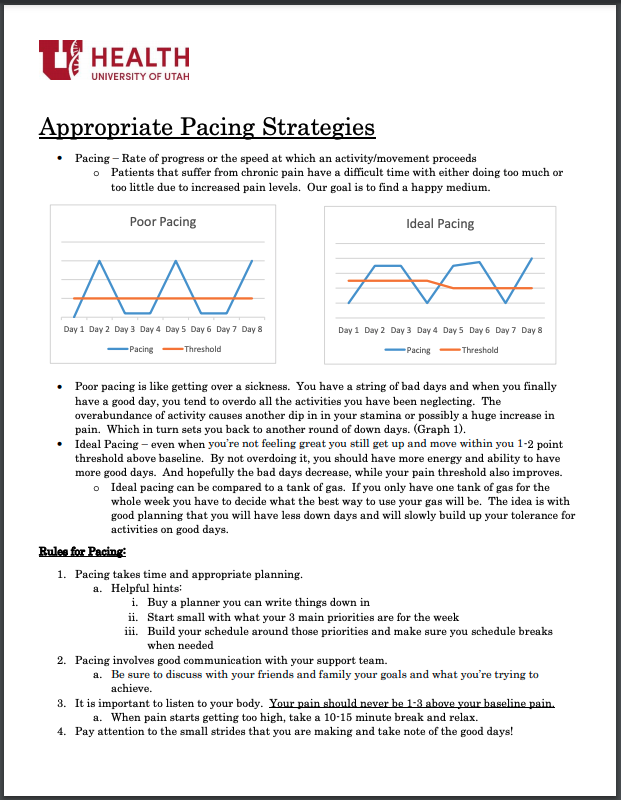
2. Pacing
People with chronic pain often have days where they're flat on their back and can't do anything. When they finally feel like they can do something, they do everything, and then they crash.
Imagine that pacing yourself is like using a tank of gas: you get one tank a week, so plan out how to use a little fuel each day. Select 3 priorities for the week and arrange your schedule around them. Including breaks and communicating your goals to friends and family can help with accountability
Above all, listen to your body. If you start to feel stressed, take 10-15 minutes to relax and practice some breathing exercises.
3. Exercise and stretch
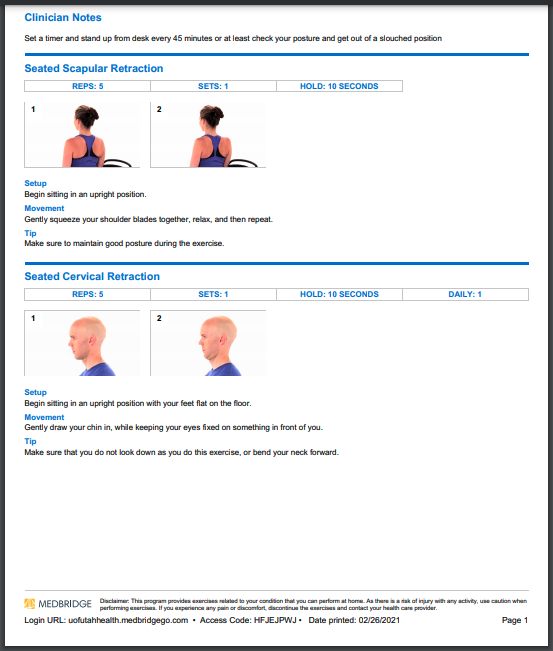
Awareness of posture and movement can also keep chronic stress at bay. Little choices like setting a 45-minute timer to get out of your chair, or occasionally checking to make sure you are not slouching can make a difference.
Simple exercises like these can also reduce pain:
-
Sit in an upright position. Squeeze shoulder blades together, pause, and release. Repeat five times.
-
Begin in an upright position with feet flat on the floor and eyes straight ahead. Draw your chin in towards your neck, pause, and relax. Repeat 5 times.
-
Using one hand, gently tilt your head sideways until you feel a light stretch in the opposite side of your neck. Hold for 30 seconds and repeat on the other side.
For more instructions, click here.
Chronic or not, we’re all feeling the stress of Covid. I remind my patients to give themselves credit for the little things right now—we all deserve a pat on the back. Taking a moment to just breathe can help you manage that pain and anxiety.
Originally published April 2021
Tasha Olsen
The U of U Health Resiliency Center shares a growing list of resources you and your team can use to continue building resilience together.
Pause practices are frequently used in the medical setting immediately following a traumatic event. The Resiliency Center’s Jean Whitlock shares a pause practice for 2020 to help teams recognize how far they’ve come—so we can all move forward together.
Taking time to reflect after a crisis is crucial for recovery. The Resiliency Center’s Jean Whitlock shares a helpful exercise for teams to recognize and normalize their experiences, fostering a culture of well-being in the workplace.