Compassionomics: The Revolutionary Science Evidence that Caring Makes a Difference, by Stephen Trzeciak and Anthony Mazzarelli.
medical students, we frequently discuss how burnout negatively impacts a provider’s life, including their physical well-being, mental health, and close relationships. However, one aspect of burnout we often overlook is the profound effect that it has on our patients. Perhaps the most important thing that an emotionally exhausted provider struggles with is providing compassion—if your personal tank isn’t full, it’s hard to share with others.
During my first year in medical school in my Value-Driven Healthcare elective class, I learned about patient experience. I realized that listening to direct feedback from patients and elevating their voices gives us the best chance to improve compassion in healthcare, and I knew I wanted to be involved.
Over the summer, I completed an internship with the Patient Experience team and facilitated a book club on Compassionomics: The Revolutionary Science Evidence that Caring Makes a Difference, authored by physicians Stephen Trzeciak and Anthony Mazzarelli.
Trzeciak and Mazzarelli make the case that the presence (or lack of) compassion touches all parts of healthcare and can have profound effects on everything from patient self-efficacy to actual psychological and physiological health benefits. This is the second of a series of two articles exploring the themes of Compassionomics with practicing providers.
In the second section of the book, the authors use published data to make the case that showing compassion does much more than make patients feel heard; it actually has specific, measurable benefits. These benefits are wide-ranging, including improved physical and psychological healing, decreased pain, and increased adherence to prescribed therapy. The authors also describe how showing compassion helps providers, explaining that providers rated as showing compassion were less likely to make a major medical error in the next three months.
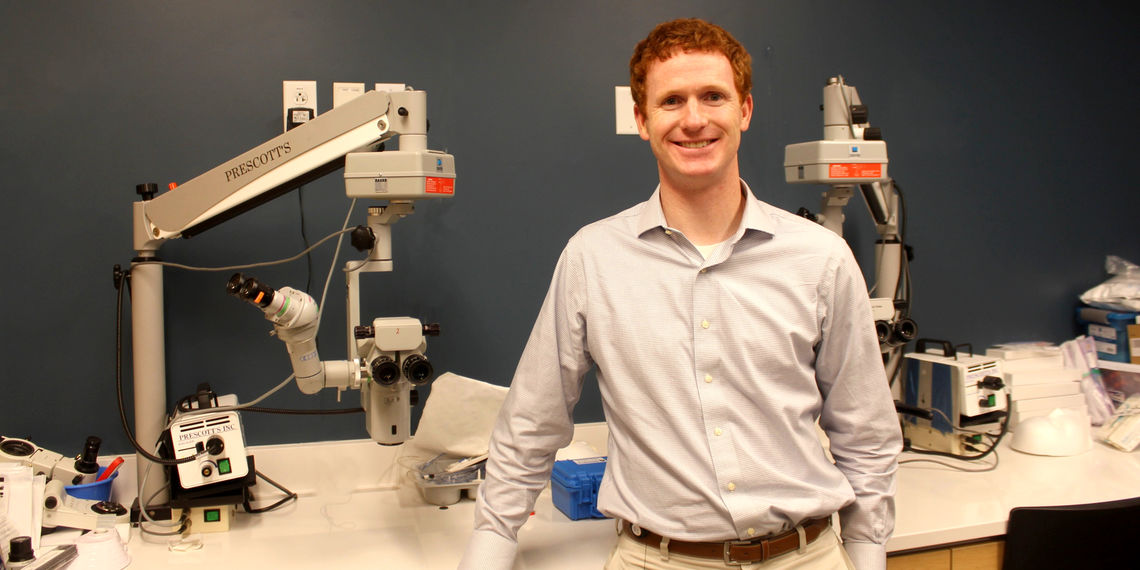
It got me thinking—how have providers at the University of Utah experienced these benefits in their own practices? Are these benefits seen in daily interactions with patients? I spoke with Griffin Jardine, a pediatric ophthalmologist at University of Utah Health’s Moran Eye Center. Griffin is regularly recognized by his patients for his empathy and compassion.
Tanner Nelson: How do you show compassion toward your patients both with and without words?
Griffin Jardine: I try to slow down to be present, to really look at my patients and read their body language. I have to really listen to what they are saying in words—and without words. Being fully involved in conversations can give us clues as to where our patients are really worried and what they are really concerned about. Their concerns may be different than our concerns, their agenda different than our own. And they won’t care about our concerns until their concerns are addressed.
Once, I was seeing a child who was severely visually impaired. I was focused on getting him glasses that could help, that could improve his vision. His mother was focused on his eye allergies, which were causing terrible itchiness. When we got him the glasses, I was thrilled that he could see so well. I thought his mother would be thrilled, too. But she felt upset that his eyes were still itchy. I missed that those were her main concerns, that those needed addressed first. Patients know you care about them when you take the time to validate their agenda and concerns before you address your own.
Compassion also stems from honesty. It comes from sincerity. When we talk with patients, we need to echo back their concerns then provide open, honest information. This knowledge can help take away some fear and empower them to take part in their care.
Patient-centered communication improves adherence to treatment
Drs. Trezeciak and Mazzarelli highlight a comprehensive meta-analysis of 127 studies that found that patient-centered communication from health providers was associated with 62% higher odds of patient adherence to treatment.
TN: You are often faced with patients and their families who are going through difficult diagnoses. How do you provide hope and compassion in those situations?
GJ: Hope can be easy to offer in some situations, when treatments are plentiful and effective. We can set good expectations for our patients and share our optimism with them.
But hope can be difficult to find, too. I have cared for patients in tough situations, such as infants born with blinding conditions or children with eye cancer. These parents can feel devastated that their child may lose their vision or never see at all.
We can’t jump to hope too quickly in these situations. First, we have to feel devastated with them. We can sit and cry. We can offer tissues and empathy. After those emotions have been felt, we can start to share hope. I can let parents know that I have so many patients who are significantly visually impaired who live meaningful, wonderful lives. I can share with them how adaptable and amazing kids are, how their brains can learn to adjust without vision. I can let them know that they, as parents, can provide all the love and support their child needs.
I still think there's almost always room for hope, and I think hope is what gets us out of bed in the morning. if we don't have hope there's nothing to move forward for.
I think so much of compassion is giving people something to hope for even in hard times.
TN: We know that burnout among healthcare providers is at an all-time high. How do you take care of yourself in order to ensure that you are providing and showing compassion toward your patients?
GJ: Compassion takes physical, mental and emotional energy. So, in order to show compassion day in and day out, we must first show compassion to ourselves by caring for ourselves. Healthcare providers in general feel like they always have to neglect their own self-care because the patient's needs are more important, but that self-care is so critical. We need to eat well, aim for 8 hours of restful sleep, get outside and get moving. We have to make taking care of ourselves a priority whenever possible.
TN: Do you think there are any barriers that might cause a provider difficulty in showing compassion toward their patients?
GJ: There are huge barriers to compassion on a system level: appointments that are too short, having too many patients, working hours that are too long. But even on a small level, in the room with patients, we can come up against barriers.
Compassion takes time, which can be hard to find when providing healthcare. If you're spending all your time on the computer and you can't look the patient in the eyes, you can’t provide compassion. We need to be working as a system to find ways to optimize our ability to feel and then express that compassion, whether that’s using scribes or AI or other techniques to increase the time we have with our patients.
Our own knowledge and experience can even prevent us from empathizing with patients. We may have seen a diagnoses a thousand times. We may know that the treatments are good. But our patients don’t. This is new to them, it’s personal to them. We have to stay empathetic and remind ourselves that each patient is in new, unfamiliar territory for them.
We also have to be mindful that emotions like fear, worry, or anger can be contagious. And in healthcare, we meet a lot of worried and afraid people. Unfortunately, their feelings can rub off on us and make compassion more difficult. When patients yells because they are scared or frustrated, we become frustrated, too. When they get flustered, we can get flustered, too.
Furthermore, we often project our own insecurities on others. We can get defensive when someone asks how many surgeries we have done or how old we are. We want to defend our qualifications. But when we are in a defensive state, our ability to show compassion is compromised. It’s happened to me. It happens to a lot of providers.
When we keep our voices calm, optimistic and understanding; that too can be contagious and help establish a therapeutic relationship with patients. It can help steady them as they navigate their emotional and physical health challenges.
TN: Do you believe that compassion provides a therapeutic benefit and that it can actually improve someone's condition physiologically, as well as have a decrease in medical errors among healthcare providers?
GJ: The compassion we can show our patients is beyond a tangible experience, it is beyond words. It has a power to health that’s not from treatment or intervention, but from connection.
When patients feel that you have a genuine interest in them and their wellbeing, that compassion can absolutely have a therapeutic benefit.
Aside from the benefits of feeling seen and heard and cared for, genuine compassion can improve the quality of care we provide for our patients. For instance, in the OR, there are numerous distractions from people going in and out of the room, overhead pages, machine sounds and so much more. But compassion keeps us rooted in the moment, focused on the person we are caring for. When we achieve that focus, we can reduce our rate of errors from all those distractions.
TN: There's a Teddy Roosevelt quote in the book that says that people don't care how much you know until they know how much you care. Do you agree with that?
GJ: Yes, I do agree with that. Patients know you care about them when you take the time to validate their agenda and concerns before you address your own. Patients won't care about your agenda until you validate, listen and speak to their agenda.
I think everybody who goes into healthcare already has the built-in ability to be incredibly compassionate. And I think everyone knows, and the scientific evidence shows, that compassion benefits our patients’ health and wellbeing. We can have every treatment in the world, all the data to back it up, but we need to pair those treatments with compassion every day for great patient outcomes.
How it feels for patients
Dr. Jardine is an incredible doctor. Absolutely perfect with children. He genuinely cares, works quickly, and maintains comfort through the process. He made the appointment fun for my daughter. She wasn't nervous when he made her appointment about "play". She still talks about being magic! He took time to describe her condition and what to expect best case scenario and worst case scenario. He made sure I knew the treatment plan and what needs to happen moving forward. So so good!
I absolutely loved Dr Jardine. I was worried about how an eye exam would go with a highly uncooperative one year old but this doctor was so fantastic. He had so many tricks up his sleeve to get my son to cooperate. I was so impressed with his bedside manner, both with me and my son. He went as far as using my phone to take pictures of my son's eyes to help me visualize exactly what he was talking about. He was so great and I'm so grateful to him for easing my concerns.
Dr. Jardine is a spectacular doctor with a concerned and very kind support staff. My son had special needs, and every one of his care providers was kind and respectful and made a clear effort to include him in all the interactions, even though his speech is limited. I knew Dr. Jardine had a large number of patients stacked up to see after (patient name), but he took all the time necessary to address (patient name’s) case and go over our options regarding surgery. He's an excellent ophthalmologist and you are lucky to have him on staff.
Griffin Jardine
Tanner Nelson
U of U Health's Patient and Family Advisory Council and Advise Utah recently gathered feedback from patients and caregivers on inpatient surveys and communication. Patient Experience's Corrie Harris, Marcie Hopkins, and Shayma Salih share insights from these advisory councils.
Negative self-talk lurks as a formidable threat, silently undermining our confidence and stifling our potential. Recognizing its dangers, Leadership Training Specialist Jess Burgett equips us with essential strategies to combat unhelpful internal dialogues, turning our thoughts into powerful allies for a more positive and successful life.
In this first of three articles, University of Utah Health’s Chief Executive Officer Dan Lundergan shares how the same core values and beliefs that carried us through the pandemic will continue to successfully carry us into the future.