The Distraction Study: National Impact
After the implementation of the central call center, employees at the community pharmacies reported improved teamwork, better communication about mistakes, improved pace of work, and increased ability to learn at work. These findings, now published, are making their way into the national conversation.
Am J Health-Syst Pharm (2019)
you’ve visited one of University of Utah Health’s 16 retail pharmacies in the last few years, you might have noticed something: (relative) tranquility. Pharmacists and pharmacy techs speak with patients, analyze drug interactions for every patient, and solve problems together. If you look closely, you may even see a robot filling 200 of the most commonly prescribed drugs.
All of this is happening without something we’ve become accustomed to in busy offices or clinics—ringing phones. This is the result of years of work re-envisioning what the practice of community pharmacy feels like, both for ourselves (the employees) and for our patients.
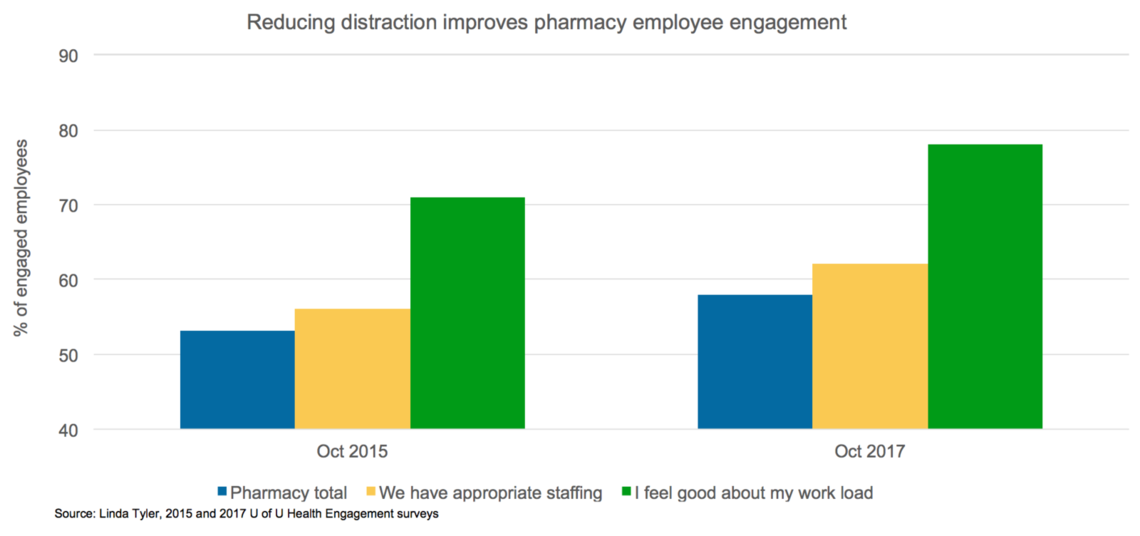
In 2015, we set out on a multiple year journey to improve safety and reduce medication errors through a unique approach: reducing distractions. We’ve found that reducing distractions has the added benefit of increasing employee engagement. That’s partly because employees now spend more time doing the work they find meaningful: keeping patients safe.
Here are four insights from our work to reduce distraction.
Expand your team
How distraction impacts inpatient care is widely studied, but there are few studies that explore distraction in retail pharmacy. We partnered with researchers in the psychology department to create the “Distraction Study,” which is the umbrella for many pharmacy culture and safety projects.
The premise for the distraction study is that we can create a safer environment by decreasing distractions.
 One of the benefits of working in academic medicine is access to researchers from across campus. We were thrilled to find that we had an expert in our own backyard. University of Utah psychologist David Strayer is nationally recognized in the study of multi-tasking and human attention. His research made it into popular consciousness when he showed that being distracted while driving is equivalent to being drunk while driving.
One of the benefits of working in academic medicine is access to researchers from across campus. We were thrilled to find that we had an expert in our own backyard. University of Utah psychologist David Strayer is nationally recognized in the study of multi-tasking and human attention. His research made it into popular consciousness when he showed that being distracted while driving is equivalent to being drunk while driving.
We were also fortunate to work with human factors expert Frank Drews of the psychology department, who has collaborated on many safety efforts at U of U Health.
Special thanks to professor of pharmacotherapy Nancy Nickman who coordinated data collection and publication of papers. We would not have been able to sustain this project without her.
Balance quality with service: Centralizing calls, refills, and robots
As pharmacists, we want to take care of our patients by ensuring that the medications they take aren’t contraindicated. We also ensure patients are getting therapeutic benefits from their medications and that they can afford them.
Answering phones, filling prescriptions, and then checking and double-checking the work takes away from those important patient-centered conversations. We decided that we could free up time for those conversations by centralizing some of the time-consuming functions that were being done locally in each of our retail pharmacies.
It was critical for us to ensure that by centralizing functions we didn’t lose sight of what was important to the patient. That is, we wanted to make sure we were providing the same level of service, or better, that they were used to at their local pharmacy. If we had a central place where calls were taken and prescriptions filled, would patients still feel known?
Centralize calls—peace comes to the pharmacy
We decided to centralize calls and were surprised at what we found.
One of us (Russ) was managing University Hospital’s Outpatient Pharmacy, and we didn’t think the change to a central call center would really impact us. But the day that the calls switched, it was like peace had come to the pharmacy. Before, technicians answered most of the incoming calls, but those techs were also doing important tasks that would be interrupted by incoming phone calls. You would feel this frenetic movement – people running back and forth.
"...we didn’t think the change to a central call center would really impact us. But the day that the calls switched, it was like peace had come to the pharmacy."
Now the central call center answers 15,000 to 16,000 calls a month. That reduction in calls to the community pharmacy has corresponded to an increase in meaningful patient interactions. Patients have noticed that the phones aren’t ringing off the hook.
Decreasing call volume has also improved team culture. Techs feel like they can ask the pharmacists questions. They have time to talk to each other now. According to engagement study results, team cohesion improved in year one after the call center was implemented.
Centralize refills—streamline the work
During our second year, we began a central refill center in Midvalley. At first, we started the big pharmacies on central refill. Behind the scenes, when someone puts in a refill request, the system automatically routes the refill to the central center, the central center fills it and delivers it. We actually get better delivery times than what we were able to do when we filled it in the pharmacy.
By concentrating that work in one place, it just really streamlined the work in pharmacies. Many of our pharmacies are in fairly cramped spaces, so by offloading that work it helped decrease some of the distractions and increased the capacity of our system to fill prescriptions.
Preventable errors—automation improves safety
We have installed robots at many of our pharmacies. These robots fill the 200 most common medications. At our Midvalley location, we have a two high-capacity (soon to be three!) robots. Midvalley is also home to our high-capacity mail order center. From the start of the process to the time it leaves the pharmacy, we've got barcode scanning every step of the way.
Automation has allowed us to have safety checks at every point of the process. We can ensure that the right prescription gets to the right patient in a timely way. It has helped us become more efficient AND safe.
Use data to avoid unintended consequences
We knew it was important to understand the full impact of the changes we were implementing. The one thing we hoped to avoid was to make a major change in the pharmacy that would result in a negative change to our culture of safety.
The “Distraction Study” has been a really incredible process in terms of how we think about safety and engagement–how we measure it, talk about it, evaluate it. We think it’s been really important for all of our staff to know that we care about this.
We care about measuring it. If we’re finding opportunities, we want to capitalize on those opportunities to create the safest environment for our patients. But that also translates to a better working environment for all of our staff, and that’s all important.
"The 'Distraction Study' has been a really incredible process in terms of how we think about safety and engagement–how we measure it, talk about it, evaluate it."
We’ve taken the angle of using a very broad range of tools to understand the impact the changes we make have on patients and the pharmacy team. To that end, we don’t just measure safety, but we look at employee engagement and other metrics for understanding workload. The Nasa Task Load study, AHRQ, and our own employee engagement survey have all been crucial tools for measuring our efforts.
Reduce Rework
We’re counting errors, and in our world, that is called "rework." In all of our pharmacies, we have a "bench." Prescriptions come in at one end of bench, technicians input it, answer questions, and work with the patient’s insurance company. Then, the pharmacist checks it to make sure everything is correct.
Once the pharmacist checks it, the technician prepares the medication. Next step on the bench is a second pharmacist to check the medication for accuracy. If it gets to the end of the bench and the pharmacist catches an error, they send it back to the beginning of the bench.
That process is rework. In some places, it used to be as high as 15-20%. But our process changes—central calls, central refills, automation—has significantly reduced reworks.
Reflection: More efficient service to patients, better work for employees
More than half of Pharmacy’s 800+ employees are employed in retail/ambulatory care/community pharmacy area. When you think about the number of people impacted, we hope we made the changes feel invisible. You don’t know your prescriptions are being filled someplace else or that your phone calls are being answered someplace else. You know that your calls are getting answered faster and you’re getting to resolution faster.
We want patients to feel like they’re in a quieter environment when having a conversation with the pharmacist. In reality, it’s not ideal—you’re standing up, talking over a counter. These are barriers to having a great conversation. But if we can decrease that hecticness found in so many of our interactions, the difference for patients is incredible.
Originally posted July 11, 2019
Contributor not pictured below: Russ Ragsdale.
Nathan Hagen
Linda Tyler
Ashley Bowden
Urogynecology specialist Whitney Hendrickson-Cahill details the steps an interdisciplinary team followed to reduce surgical site infections (SSIs) following hysterectomy procedures, aiming to improve patient outcomes, shorten recovery times, and reduce healthcare costs at University of Utah Health.
Former Chief Quality Officer Sandi Gulbransen and Accreditation Manager Kemper Funk explain how this umbrella of standards—ISO-9001—relates to our accreditation process and impacts our daily work.
Pediatric hospitalists and patient advocates Reena Tam and Erin Avondet shed light on the untapped opportunity to augment pediatric vaccination coverage in our communities and build vaccine confidence in the inpatient setting. They provide a host of resources and practical tips you can apply right now.
