PX Leader Guide
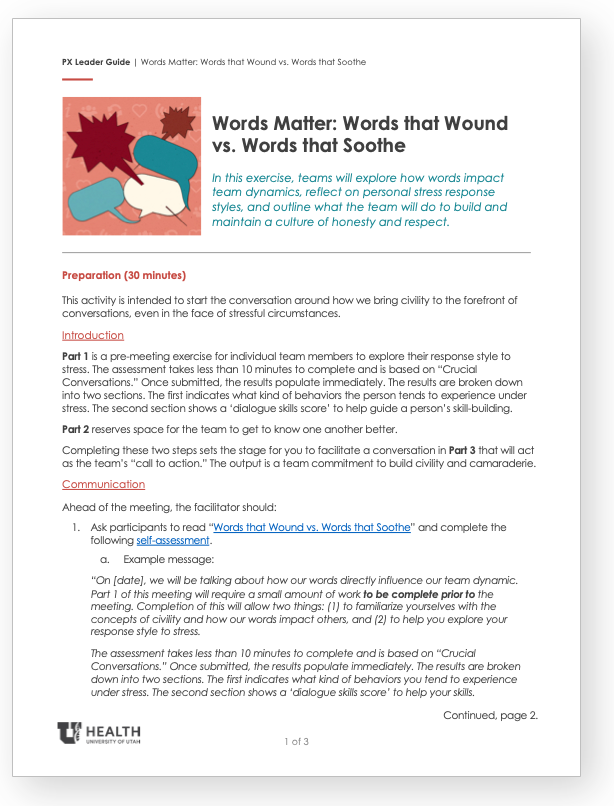
Download the Words Matter Leader Guide for a team activity that explores the way words impact team dynamics, how our personal stress response comes into play, and ways to build a culture of honesty and respect.
hether we’re comforting someone in need, or establishing a needed boundary, the choice of words we use makes all the difference. On any given day, our environment, our internal world, and our personal communication styles influence the way we choose to communicate with others.
For example, consider a time you were able to speak with a colleague, or patient, without perceived time restrictions—that time may have allowed for more meaningful conversation to unfold. Conversely, consider a time you were multi-tasking and had somewhere to be, ten minutes ago… time pressure may lead to a harsher comment, or dismissive gesture that, albeit unintentional, has the potential to negatively impact the person on the receiving end.
Sometimes our intentions, our words, and others’ interpretations of these things are misaligned.
We may intend to clearly communicate the next steps in patient’s care plan with authoritative language, and our teammates may interpret our words as uncomfortably direct, or even hostile. We may intend to quickly respond to the urgency of a situation with a clipped request, and our teammates may feel disrespected by our tone. Even a poorly timed sigh, due to our own fatigue, could be perceived by a colleague as impatient with them personally. Whether you find yourself in a heightened state of stress and irritability, or you are naturally assertive and direct in your communication style, when emotions run high, it limits our ability to choose words that demonstrate respect. If this continues to happen, it becomes our team culture.
Civil dialogue isn’t a “nice to have”—it’s necessary.
You may believe that civility matters in general, but that critical scenarios can occasionally surpass need for “niceties.” If the patient is ultimately cared for, if a life is saved, do the words we use really matter? The research on workplace civility answers a resounding “yes.” When we allow less-than-civil communication to help us achieve our goals for a patient outcome, a financial outcome, or an operational outcome, we ultimately harm our ability to deliver results in the long term. Incivility takes a mental and physical toll on employees, and disillusions patrons who witness incivility.
Five ways to bring civility to the forefront
How do we bring civility to the forefront of our conversations, even in the face of stressful circumstances?
1. Start with yourself.
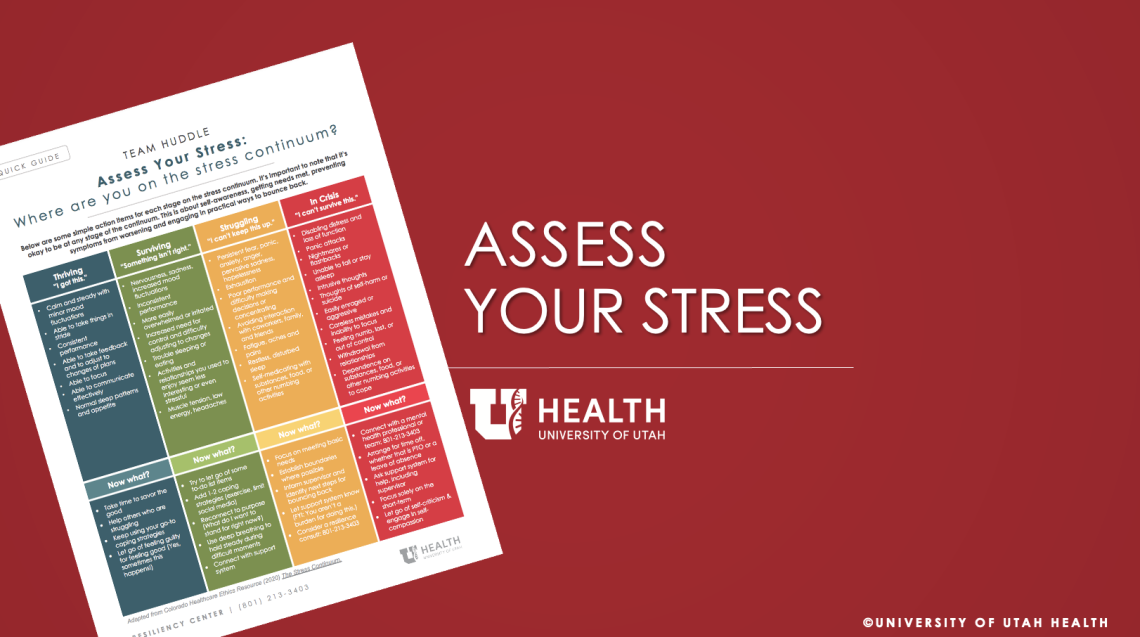
What does your internal pressure feel like? Are you about to lose it on the next “ridiculous question” that is lobbed your way? Or are you in a state where you are genuinely curious about another person’s thought process? The Stress Continuum is one framework to help you objectively assess your baseline prior to communicating with those around you. Stress can amplify our reactivity to different situations or cause us to withdraw completely from communication. Understanding what triggers our stress, and how we respond, helps us speak and behave more intentionally.
2. Shift your focus.
It is easy to get swept up in our own thoughts and daily tasks. Stopping to consider where others are emotionally and mentally plays a key role in our willingness to use considerate language. Do you know your colleagues well enough to gauge where they are emotionally? Do you want to? Asking these questions can help create self-awareness and shift your mindset to focus on another person’s needs. If you know someone is going through a challenging time in their personal life, you may be more likely to give them the grace they need through the words you choose.
3. Commit to Honesty and Respect.
WE CARE: RESPECT
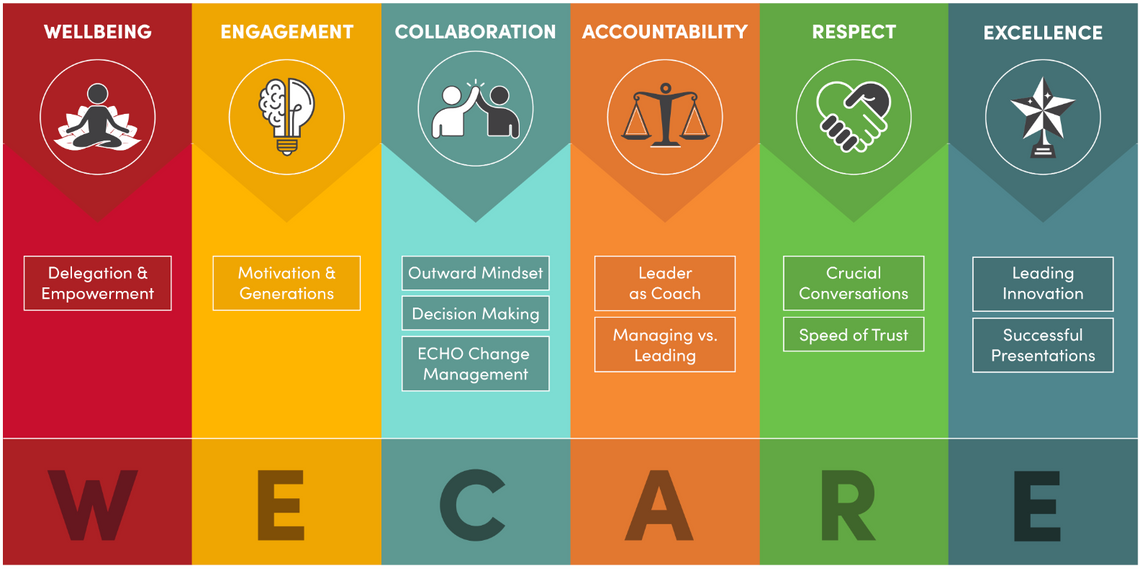
U of U Health Hospitals & Clinics leaders can sign up for training in Crucial Conversations with Jess Burgett.
It’s common to assume that we can either be direct or we can be kind, but not at the same time. This false dichotomy, and how to avoid it, is explored at length in Crucial Conversations. Thoughtfully, gently, and clearly sharing our genuine concerns is one of the kindest things we can do for our teams. Commit to being both 100% honest and 100% respectful; if this feels daunting, check out this course on Crucial Conversations.
4. Build Camaraderie.
Creating an environment where individuals fully trust one another and feel a sense of community is difficult and takes time. Building that camaraderie should be approached in a way that feels authentic to the current team dynamic. The following are tips to get started:
- Get to know others: Learning about others allows you to connect on more than daily tasks. The way someone reacts to stress, solves problems, or spends their free time creates space for understanding where they are coming from. It allows you to appreciate their differences, needs, and how to flex into the communication space that enables their success.
- Create shared understanding: Knowing roles and responsibilities lays the groundwork for this. Misunderstanding in these areas is what often leads to unrealistic expectations and subsequent conflict. It is important that we ask for clarification when we do not understand someone’s role or specific tasks, we believe them to be responsible for. Knowing ‘how’ to ask for clarification can help improve psychological safety and the ability to receive a more transparent answer.
- Normalize respectful “call outs.” When was the last time you felt comfortable in “calling out” a colleague for an inappropriate or unappreciated comment? When done respectfully, this can facilitate deeper trust between you. Tone, inflection, and word choice matter more than ever when emotions can run high, making it imperative that we are polite yet direct in our approach. This may look/sound like:
- During rounds, a team member loudly sighs and says: “they should know this.” Another team member could say—I hear your frustration and see that there may be learning opportunity here. Let’s come back to this topic at a more appropriate time.
- After checking a patient in, your teammate mutters something under their breath about that patient. You quietly ask, “Are you alright? I think I may be sensing some stress.” If they need to talk or take a moment to decompress, plan to support that.
5. Follow up.
Regular reinforcement is necessary. It demonstrates a commitment to building a culture of civility—where everyone is confident that they can come to work and be treated with respect. Scheduling time to talk about the “current state” of the team’s communication progress allows this type of follow-up to be prioritized. For those who are working through a "storming" phase of their team dynamic, once per week may be most appropriate, while those who are in a steady state with their collaboration may only need to follow up once per month or quarter.
Put it into Action: Words that Wound vs. Words that Soothe
Every interaction presents us with a choice on how we will speak to others. Our civility and respect have an important ripple effect in creating a supportive working environment. In allowing people to feel psychologically safer at work, we create conditions for sharing information more readily and having greater fulfillment in what we do. That level of trust has been shown to improve patient outcomes in a variety of disease states.
If trust decreases, it can come with dire consequences. A study completed by the Institute for Safe Medication Practices showed almost half of respondents indicated that they were less likely to speak up and ask questions about administering medication to patients when intimidation from their team was involved. Knowing this, we have a moral obligation to ask ourselves what impact our words are having. Taking an extra moment to choose our words thoughtfully can quite literally be the difference between inflicting injury or remedying it.
In Conversations with Colleagues:
| Words that Wound | Words that Soothe |
|---|---|
|
In front of other colleagues, you say: I’ve already explained this once, I shouldn’t have to tell you again! Other nurses know this. Why don’t you? |
Away from other colleagues, you say: I feel that you may need more support and understanding on X. How can I help with your learning? |
| Ugh, EVS never cleans well enough! I left these crumbs on the floor last week to test it and they’re still here! | I am noticing a pattern with the cleanliness of our floors. Can you help me understand how often we should anticipate them being cleaned? How can our team help to make your process easier? |
| My dad is a physician and he would never speak to someone that way. Don’t you want to be good at what you do? | I’m hearing frustration come through in the way you’re communicating. Are you alright? Are you open to talking through this with me or someone else? |
| Your job isn’t that hard, don’t you just click a button to check patients in all day? You should easily be able to take on this task for us. Be a team player. | My understanding of your role is limited. Can you help me understand X. Is there room to involve your support in a new task we need help with? |
| Following a presentation, you sigh loudly and say “oh, thank you. I thought that would never end!” | Say nothing out loud, or a simple/respectful thank you. |
In Conversations With (Or About) Patients:
| Words that Wound | Words that Soothe |
|---|---|
| Oh, <provider name> always runs late. I’m sorry about that. Next time bring a book to pass the time. | I know you’ve been waiting a while. I want to apologize for that. <provider name> is wonderful to ensure she addresses every question each patient has. She’ll take great care with you. |
| You’ve been pressing the call button a lot. We don’t have enough staff to answer this many requests and other patients are in worse shape, so you will have to wait. | I’m wondering if we can work to group your requests so that we can meet your needs. Here’s what I would propose. |
| The <provider name> told you they were going to prescribe <drug name>? Why don’t they ever tell us these things or put notes in the chart? | Sounds like the plan has changed in an important way. I'll connect with <provider name> to collaborate next steps. |
| I can’t prescribe that antibiotic for you. You’ll just have to wait it out. | I hear your request for <antibiotic name> and recognize that it has worked well for you in the past. With where you’re currently at in your illness, it’s not yet appropriate to prescribe this. |
| Room 204 is wanting more pain medication. They’re the addict that came in last night. | The patient in room 204 is having increased pain. I wonder if we want to offer alternative measures or provide more medication. |
|
In the waiting room, you say Ugh, <patient name> is so mean! Every time she comes here she fights with me when I ask to verify her demographic information. |
Say nothing out loud or check with a colleague if they can cover for you while you take a 5 minute break to decompress. |
Ember Hunsaker
The patient experience team shares resources to build coordination and teamwork centered on the needs of patients, caregivers, and families.
What do patients want? University of Utah Health’s patient experience team reveals what fifteen years of evolving qualitative analysis of hundreds of thousands of patient voices have taught us.
Patients experience multiple handoffs, or transfers of care, during their visits, surgeries, hospitalizations, and scheduling. Every handoff is an opportunity to demonstrate trust and safety. Utah’s Patient Experience team shares universal best practices to apply.