The Weak Spot
just received a call I’ve had many times, a harried physician calling “to improve my patient satisfaction.” In this case, the caller is a surgeon who I know well. He has cared for my family member over several surgeries. I know this physician to be an excellent communicator — caring, great listener, gifted teacher who explains thoroughly and carefully. The weak spot: wait times that are legendary. Over the years, I’ve spent hours in the waiting room with other patients. Can exceptional bedside manner make up for an exceptional wait time? If anyone can provide a test for this hypothesis, this is the physician.
This provider deeply respects his patients. But what about the systemic disrespect of waiting? Waiting is such a firmly entrenched feature of healthcare that it is often taken as a given and not recognized for the disrespect it conveys. Wait time sends an unambiguous and often unintended message that the physician considers their time more valuable than the patient’s. So what would the numbers say?
On our patient satisfaction surveys, patients self-report the number of minutes they wait in the exam room for the provider. For this provider, we pulled 567 surveys and grouped them by patient reported wait times: < 5 minutes wait, 6-15 minutes wait, and more than 15 minutes wait (that included waits beyond 60 minutes). Here are the results:
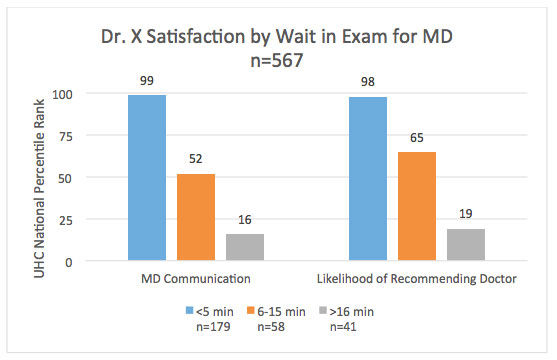
As you can see, it really is a tale of two experiences. When the system works, and waits are minimal, this provider is providing an exceptional experience to his patients. But as the clock continues to tick, the same physician is perceived very differently. Intention isn’t perception. Wait time matters.
How they fixed it:
The solution for this physician came from teamwork and template design. When the team looked at the data, they discovered two things: 1) About 25% of patients wait more than 15 minutes, and 2) about 25% of patients were added on each day. The MA identified that every patient has three post-op visits, two of which were scheduled at the time of surgery. Because the provider was very in-demand and almost always has a third post-op visit, these appointments were always add-ons. The manager is now in the process of integrating the third post-op visit into the standard schedule, reducing the number of add-ons.
How you can fix it:
As a system, we have seen that when we reduce wait times, our providers as a system have become better communicators. Wait time is managed through an accurate template and a coordinated team effort. Great news: we have experts here to help. If you’re not sure about your wait time, start with your clinic manager, partner with the template optimization office, and engage your MA staff to help.
Chrissy Daniels
University of Utah Health’s director of patient experience Mari Ransco examines the pandemic patient experience through the lens of the 5 Elements: U of U Health’s qualitative model for delivering an exceptional patient experience.
Patients will ask three things of us over the next decade of health care improvement: help me live my best life, make being a patient easier, and make care affordable. To meet those needs health care must shift—from organizing around a patient’s biology to understanding the patient’s biography.
Virtual care is the way of the future. How do clinicians trained in a face-to-face world transition their skills for a virtual care environment? Physician assistant Jonathan Chao shares three ways Urgent Care delivers expertise and compassion in a virtual world.
