Tell me about your team – who’s on it, what do you do?
Our team, led by outpatient nurse Laurene Vickers, includes nurses, medical assistants, radiation therapists, doctors, and members of our medical physics and dosimetry teams. Through shared governance, we have enhanced communication, refined documentation practices and established team goals, such as improving our patient experience scores by effectively managing handoffs and introductions.
How does shared governance work within your team – do you have a board, do you huddle, how’s it going?
Physical Team Board: We have a physical board located in our nurse workroom.
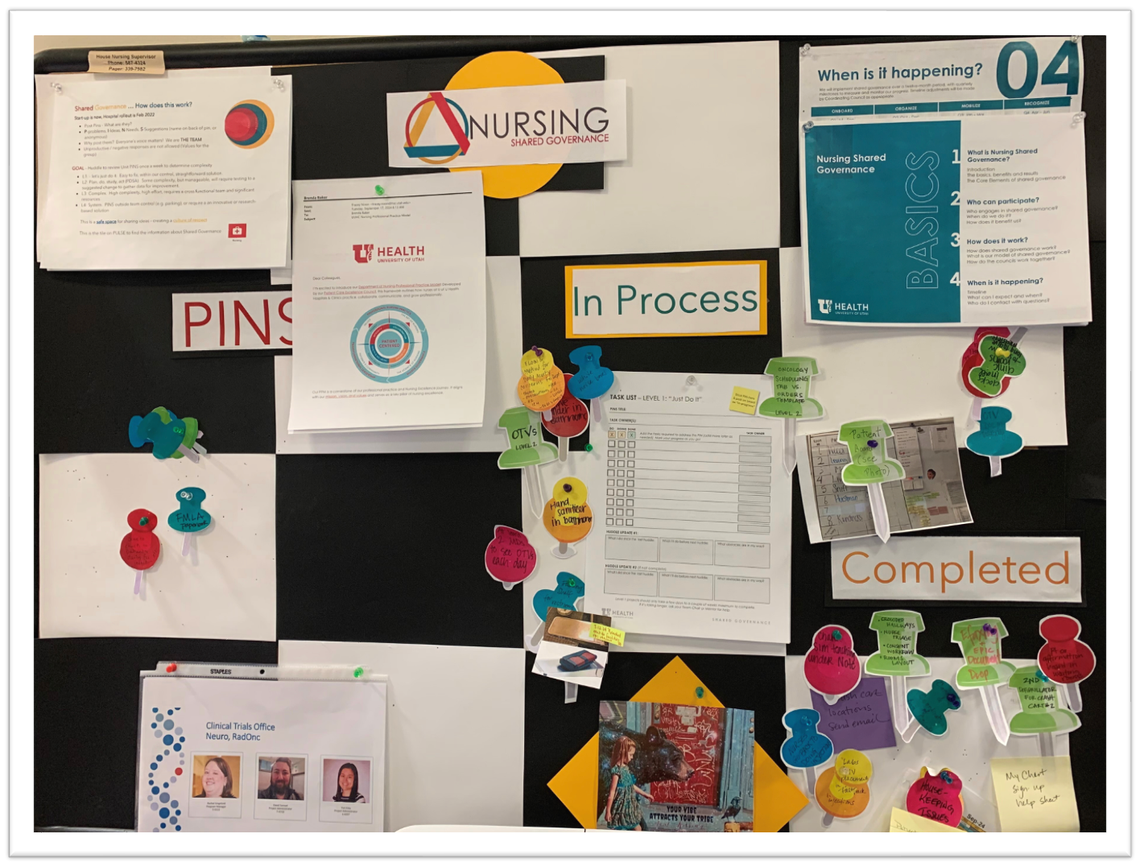
How We Huddle: Huddle is held in person every Tuesday @ 3:00 pm to review PINS that have been posted throughout the week. All Radiation Oncology team members that are interested in participating or have posted PINS are invited to attend. We review PINS as a group, then decide if each one is something we can address as a team or should be advanced to local management (Level 2) or the Coordination Council (Level 3).
Can you provide an example of any exchanges around problems, ideas or needs that people had to decide as a group or collective whether or not to work on it?
We are an ambulatory department within a hospital that performs multiple procedures and sees patients daily for radiation treatment. Due to a disconnect between two documentation software programs, encounters were not transferring to patients' MyChart. Instead, they were classified as documentation rather than patient visits, preventing our patients from accessing their treatment visit (OTV) notes and placing us out of compliance with DNV.
The problem was identified by a new procedural nurse, Paige Stringham. She posed the solution to work collectively on implementing Epic support around restructuring documentation. We partnered with nursing informatics, IT, anestesia, and the HCH PACU, to restructure our entire documentation process, and transitioned from an ambulatory department to a hospital outpatient department in Epic.
What impact (if any) has it made on the team?
The go-live occurred in September, and while we implemented a few workarounds to address minor bugs, the transition to a more robust EMR has been largely successful. This upgrade supports our work and enables our patients to access their information after each visit.
We want to hear from you!
Want to share your team’s story? Click here or email Bridgette.maitre@hsc.utah.edu to set up a Microsoft Teams discussion.
What we’ll need:
- Pictures of your team and team boards
- A picture of you – the contributor!
Brenda Baker, BSN, RN
Health systems across the nation utilize shared governance programs to empower teams to make decisions impacting their practice and area of work, increase accountability and autonomy, and improve quality of patient care. The U of U Health Department of Nursing offers its model, along with tips, to assist any team in implementing shared decision-making in their respective areas.
As teams across the UUHC Department of Nursing work to implement shared governance in their areas, we’re learning about team experiences and the impact shared governance has had so far. This month, Lauren Studiner from HCH 4B shares how shared governance helped her team overcome workflow challenges and create a more inclusive culture around idea-sharing and decision-making.
The Shared Governance Support Team has developed a list of resources for new shared governance leaders to equip them to lead and guide team members in engaging in shared decision-making at the local level.
