hen I came to the United States from South Korea in 2004, I wanted to get an MBA and go into management. I was at UCLA completing my pre-MBA courses when my plan changed. I realized I wanted to impact people's lives.
Trust was most important to me. I saw a Time magazine article published around 2005 that said pharmacist was the most trusted profession in the United States. Not just in health care, either—out of all professions, people place the most trust in their pharmacist.
I came to Utah for my pharmacy residency and Chief Pharmacy Officer Linda Tyler was my residency director. After I completed my residency, I was hired to create a team to centralize some pharmacy operations at what is now known as Pharmacy Ambulatory Clinical Care Center (PAC3). PAC3 helps patients throughout the system by filling medications, working with insurance companies, and authorizing refills.
Someone to trust: Supporting recently discharged patients
Beginning in 2015, our pharmacists started supporting patients discharged from University Hospital. Patients often leave the hospital with a special medication regimen. If they need help or take their medication incorrectly, they tend to come back to the hospital and are readmitted with the same complaints that resulted in their original hospitalization.
Utah’s Care Navigation nursing team also wanted to help patients transitioning from hospital to home. Natalie Manolakis and Jean Tealey contacted us about improving the process for Community Clinics patients discharged from the main hospital. The goal was to address 30-day readmission rates, so it was the perfect time to team up and collaborate.
Nursing and pharmacy split the tasks: nurses make sure the discharged patients get everything they need for follow-up visits and instructions on managing their care at home. Pharmacy helps with medication needs: verifying the new medication, as well as education about how to take it properly. We each document our encounters with patients and make sure that documentation gets to the primary care physician for follow-up visits.
Could we predict readmissions?
Matt Rim presents readmission project with Decision Support's Jeff Young at the April 2, 2018 U of U Health Leader Development Institute in Salt Lake City, Utah.
We had been working on transitions of care for about a year when I attended a conference in Las Vegas in December 2016. I saw a presentation on the LACE IndexThe LACE index identifies patients at risk for readmission or death within 30 days of discharge. It incorporates four parameters: "L" for length of stay, "A" for acuity of admission, "C" for co-morbidities, and "E" for the number of ED visits within the last six months., a broadly adopted predictive model. The index is designed to reduce hospital readmissions by identifying at-risk patients.
Under the process that existed at the time, we didn't have a standardized way of determing which patients really needed our help. Pharmacists would review each patient discharged the previous day and triage according to their understanding of the patient’s complexity. To make an impact, what we really needed was the ability to identify those patients most likely to come back to the hospital.
One month after the conference, I contacted Tony Clawson—Pharmacy’s liaison in Decision Support—to see if implementing the LACE Index at Utah would be possible. At the time, I didn't know Jeff Young and his team were already thinking about predictive analytics. When I explained what I had learned, Jeff’s team began building a LACE Index tool to help us prioritize our work each day by identifying which patient was most important to call.
Motivating the team to work together
That’s when the real work began. At PAC3, we have a team of 12 pharmacists, including supervisors, but only one pharmacist FTE is allocated for discharge follow-up phone calls. We use a flexible team approach and rotate our PAC3 staff. Everyone on the team is capable, trained, and highly engaged.
When I approached the team about this project and what we wanted to achieve, everyone agreed to the vision—we should prioritize our work and provide the highest level of assistance to those patients who most need pharmacy support. I asked the team for their help in developing the final workflow. Jeff's team helped along the way, and just three months after our first meeting, we implemented the new process.
The results
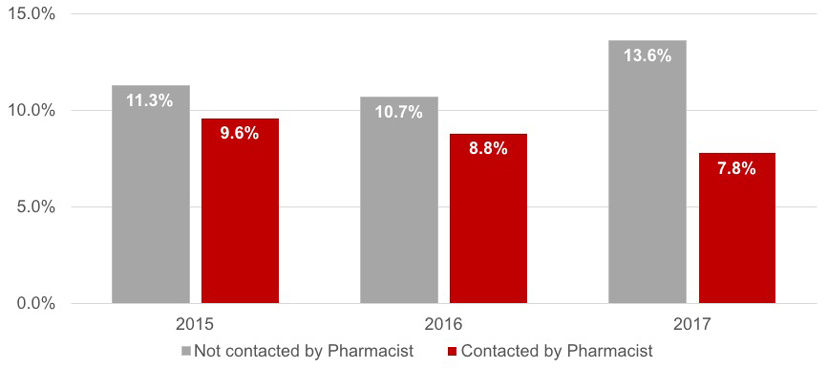
Now, the pharmacist receives an automatically generated, which lists discharged patient information and readmission risk score. The newly included information is vital for prioritizing daily work. We’ve been using the new method for one year now and have observed that the calls are making a difference. We address the problems that lead to increased readmission and help those at highest risk. So far, we’ve prevented 113 people from being re-admitted.
Reduction in 30-day readmission
It’s about trust. We value the trust that patients and other providers place in us. University of Utah Health is innovative and passionate about exceptional patient care. Our pharmacists call patients about more than just the medications. We ask detailed questions to fix any problems. Most importantly, we genuinely care about our patients.
This new process has helped us take that care one step further. When teams have the right priorities, the right focus, and the right resources, we can do amazing work.
What I learned: The formula for transformation
"Laying out the goals or outcomes you want to achieve before you start an improvement project is important. As an organization, we were already trying to reduce readmissions, so the timing was perfect when I started this project to address transitions of care. We had a VISION to reduce readmission rates, we had the right TEAM of teams that included Pharmacy, Care Navigation nursing, and Decision Support. We had a PATIENT -centered approach that targeted our highest-risk patients first. And we had a MEASUREMENT focus using the LACE Index score to prioritize with baseline rates of readmission to gauge our progress over time." –Matt Rim, Manager, PAC3
Annotated transcript from Matt Rim's presentation at the April 2, 2018, Leader Development Institute in Salt Lake City, Utah.
Matt Rim
Practicing are recorded conversations with a colleague that are shared with the organization. They are conversations between real team members about why the work matters.
Research* shows that nurse leader rounds improves a patient’s experience. This practice remains high on the list of manager “must-do’s.” But where to start, and how to keep going? Nurse Managers Melinda Patterson and Jane Nielsen share their practical approaches to moving this idea into action.
Hospitalist Ryan Murphy and Value Engineer Luca Boi outline four questions to address at the outset of any improvement.
