istakes happen. Even in a system well-regarded for quality and patient safety, medical errors resulting in injury or death do occur in our facilities. We all ultimately play a role and sometimes it’s difficult to know where to start. One simple concept that we can apply immediately is designing our work processes to keep patients “three steps from harm.” David Marx shared this concept at U of U Health a few years back.
Stay "3 steps from harm"
Here's the idea. “3 steps from harm” are processes designed to protect the patient from at least three errors before harm occurs.
Consider an everyday example: crossing train tracks. The potential harm is to be struck by an oncoming train. While the task is simple, there are many steps to prevent being struck built into the process. Physical barriers exist to prevent a person from walking across the tracks when a train is coming. There are flashing lights as well as horns to alert a person. Finally, the operator is positioned within the cab to have a good view of the path ahead with the ability to stop the train when a hazard exists.
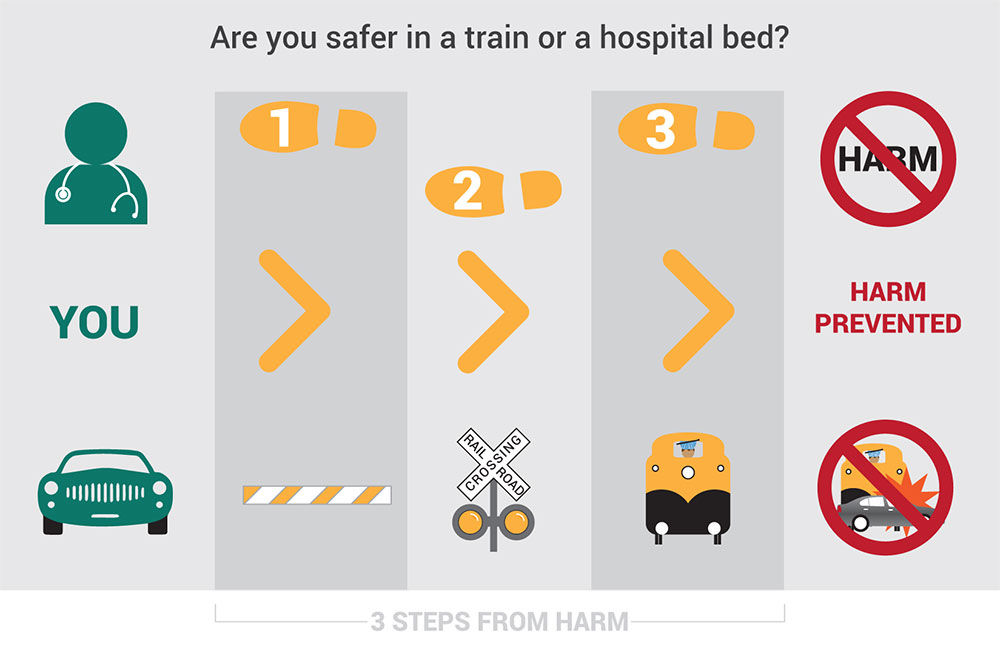
In this system, there are at least three steps or barriers protecting against a train/pedestrian impact. All three would have to individually fail for harm to occur.
See it applied: “3 steps from medication error”
Applying the “3 steps from harm” concept to real-life patient safety events isn’t hard to do. Let’s explore a medication error example from our deep library of patient safety lessons learned.
Case Study – “Beatrix and the barcode”
|
Beatrix was admitted to U of U Health for knee replacement surgery. Her nurse was busy getting other patients ready for discharge and wanted to give her pre-op medication on time. In a hurry, the nurse did not use the barcode medication administration (BCMA) technology to scan the patient’s identification (ID) wristband, or the medication barcode before administering it to the patient. After giving the medication to Beatrix, the nurse scanned the patient's ID band, the medication package, and was alerted by the Electronic Medical Record (EMR) that the medication was for the wrong patient. Beatrix developed tachycardia and hypertension resulting in a transfer to intensive care for cardiac monitoring. This wrong-patient medication error delayed her surgery for two days. Beatrix made a full recovery and was discharged home after her knee replacement surgery. |
What are "3 steps" we missed?
|
We have many practices to prevent medication errors. The standard is to use BCMA, but we can stay three steps from harm by performing the six rights of medication administration and tracing the line (at a minimum) every shift.
|
Mistakes will always happen and safety events occur. One simple concept that we can apply immediately to manage the tough leadership calls associated with holding people accountable is “Console – Coach – Sanction.” Learn all about it here.
Where can you apply "3 steps from harm"?
Think about the processes in your local work area.
- What are the steps you take?
- What can potentially go wrong within each step?
- What are the consequences if a step fails?
- Are there three steps protecting your patient from harm built into the process?
- What additional barriers can I add to ensure three steps exist?
Deborah Sax
Raelynn Frederickson
Patient safety nurse coordinators Raelynn Fredrickson and Deborah Sax share another essential patient safety concept in honor of national patient safety awareness week.
For National Injury Prevention Day, Spencer Steinbach, Senior Nursing Director, discusses safety and injury prevention in nursing and the outdoors and shares tips for your next adventure.
Kim Orton, Pediatric Clinical Nurse Coordinator for Epilepsy within the Division of Neurology, shares some insights on what it's like returning to the workplace and how we can keep each other safe.
