Quick Guide
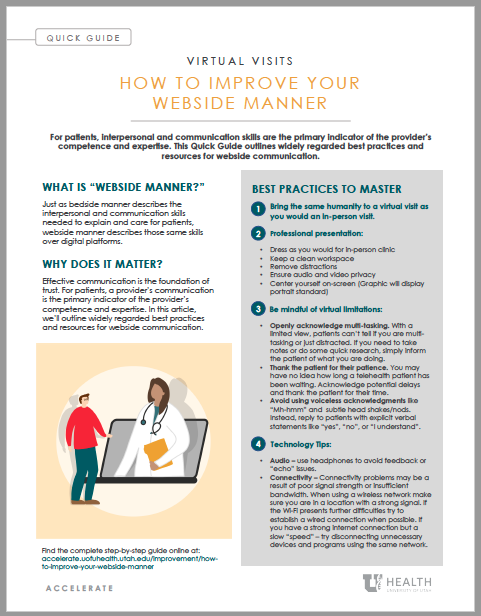
This quick guide outlines widely regarded best practices and resources for webside communication.
What is “webside” manner?
ust as bedside manner describes the interpersonal and communication skills needed to explain and care for patients, webside manner describes those same skills over digital platforms.
Why does it matter?
Effective communication is the foundation of trust. For patients, a provider’s communication is the primary indicator of the provider’s competence and expertise. In this article, we’ll outline widely regarded best practices and resources for webside communication.
Virtual presentation
-
Professional dress: Wear the same attire you would wear in-clinic. Lab coats, ID badges and other professional attire are important visual cues patients use to identify health care providers.
-
Clean workspace: Make sure the space within the patient’s view is clean and free of clutter. Remove visible food and drink.
-
Remove distractions: Hold your virtual visits in a static location without any through traffic. Mute music, television, and other unnecessary media. Avoid spaces with moving objects, active screens, or distracting décor in the background.
-
Promote privacy:
-
Secure space. HIPPA compliance requires a closed off and secure environment. This includes keeping visible windows and doors closed during visits.
-
Prevent intrusion. Make sure children, family, and pets cannot access your workspace while any patient information is being communicated or viewed.
-
Wear headphones. Wearing headphones sends a message to patients that only you can hear them.
-
-
Center yourself on-screen: Adjust the camera or change your body position. Most virtual interactions look best when following the “portrait standard,” with your shoulders at the bottom of the frame and some open space above your head.
-
Examine the lighting: Low light levels lead to poorer video quality while strong backlights often shadow your face and create a strong silhouette effect. Situating soft, direct lighting in front of you will achieve the best results.
-
Avoid motion blur: Slow your body movement and minimize on-screen activity. Stay mindful of unconscious behaviors like drumming your fingers or twirling a pen.
-
Openly acknowledge multi-tasking: Unlike a clinical environment where a patient can observe most of what you are doing, a virtual visit provides a much more limited view. Patients don’t know if you are taking notes or simply distracted. To avoid this misconception, you can inform the patient of what you are doing to keep them involved and aware.
Adapting Communication
-
Confirm a stable connection: Ask if the patient can hear you clearly and vice versa.
-
Introduce yourself: Ask how the patient is doing. Establish good-natured rapport by exchanging pleasantries and acknowledging everyone present on call. There may be additional family or staff attending the visit in a support role. Make sure to maintain HIPAA compliance when discussing the patient’s needs with any other parties present.
-
Thank the patient for their patience: In-person clinics have visible traffic and estimable waiting times. Virtual spaces are different and wait times can be lengthy with few visual cues as to when the patient will be seen. You may have no idea how long your next patient has been waiting to see you. Make sure to acknowledge these potential waiting periods and thank patients for their time and understanding. This will help reframe the undesirable experience of waiting in a more positive light.
-
Listen: Allow patients to ask questions. The cadence of virtual conversation can be awkward as there may be some transmission lag. You may need to give verbal prompts to let a patient know it is alright to ask questions.
-
Avoid using voiceless acknowledgments: Examples of voiceless communication may include “Mh-hmm” and subtle head shakes/nods. Instead, reply to patients with explicit verbal statements like “yes,” “no,” or “I understand.”
-
Convey compassion: Some elements of sincerity and empathy are easily spotted in-person but may become lost in translation during virtual visits. Try to express your compassion by visibly placing your hand over your heart when communicating your concern. Verbally acknowledge sensitive emotion with statements like “I hear how difficult this is for you…” or “Take your time, I’m here to help.”
-
Clearly define goals: During each patient encounter make time to review questions and concerns to establish the most critical items to address during the visit; then follow through. As you conclude, make sure to summarize your plans and actions (e.g., calling in a prescription, sending for tests, scheduling a follow-up visit), and remind the patient of any assignments they may need to perform.
-
Collaborate with patients: Medicine has always involved the engagement of patients and providers alike—virtual visits are no different. Work with patients to help them define symptoms, track their progress, and report on any results. This type of collaboration can often make up for some of the limitations inherent to virtual interactions.
-
Let’s not “reinvent the wheel”: Engage with patients like you would in a clinical space. Virtual interactions do have limitations, but clinical reasoning, human compassion, and proven workflows translate to digital platforms with relative ease. Stick to your established practices and make minor adjustments when necessary.
Technology Navigation
-
Learn the platform(s): Train yourself on the basic functionality of telehealth programs and consult online resources for additional guidance. Training resources for platforms supported by U of U Health are available to all providers and staff.
-
Practice: Use the platform in a variety of scenarios. Conduct trial visits with other physicians, staff, or even connect to a visit using two of your own smart devices. Navigate the platform from the provider and the patient side—learn how accessibility differs from each perspective and take notes on any troubleshooting solutions you discover.
-
Orient patients: Help patients navigate the telehealth process by giving them a brief training on connecting to visits or compile a simple “walkthrough” that can be messaged to patients with their appointment reminders.
-
Have a backup plan: Unfortunately, all the practice and training in the world won’t eliminate the inevitable need for a plan A, B, and C. Technical problems will eventually arise—be ready for them. If initial troubleshooting fails, prepare a supplementary platform to pivot to. If virtual connection cannot be accomplished make sure you can reach the patient by phone.
-
Feedback or “echo” issues: There are a number of reasons why feedback occurs while communicating through audio/video programs. Many of these issues are a product of device configuration. If you or the patient are experiencing considerable feedback problems, try using headphones. Ear buds and headsets limit the microphone’s ability to recapture the audio from your device’s speaker.
-
Connectivity problems: Most connectivity problems are a product of signal strength or bandwidth issues. While you are conducting virtual visits, try disconnecting other unnecessary devices or programs using the same network—such as streaming services, video game consoles, and other systems linking to the internet. When utilizing Wi-Fi, make sure you are in a room with sufficient signal strength. Ethernet cables can be used to establish a strong “wired” connection when wireless strength is inadequate.
Best Practices
Click here for best practices for telemedicine.
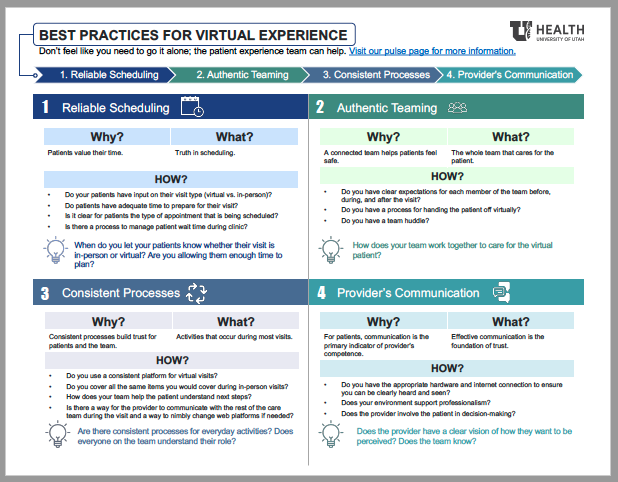
Don’t feel like you need to go it alone; the patient experience team can help. Visit our pulse page for more information.
Training Quick Links
-
U of U Health Virtual Visits Training – a comprehensive online resource for conducting virtual visits for providers and staff.
-
Additional Tip Sheets and Resources – eLearning, interpreting services, tip sheets and videos.
-
FAQ Documents – for all U of U Health virtual visit platforms.
Learn from your peers
-
Webside Manner: Three Core Competencies to Master (3 min) Physician Assistant and virtual veteran Melissa Briley shares three core competencies to master for high-quality virtual care.
-
Thank You For Being Human (3 min) – CMIO Maia Hightower, MA Eileen Prats and PA-C Christin Van Dine share how to build person-to-person human connection in virtual visits.
-
How to Rapidly Become a Virtual Clinician (3 min) – Veteran virtual clinician Jonathan Chao and new virtual provider Karly Pippitt share their experiences with what works.
-
Designing a Virtual Clinic Workflow that Actually Works for Your Team (4 min) – Neurology CVO’s Susan Baggaley and Vivek Reddy share rapid developed a new virtual visit workflow.
-
How to Lead a Remote Team (3 min) – Remote work veteran leaders Karen Wilson and Dawn Newberry distil it down to three ways to build and maintain team connection.
-
How to Lead Virtual Meetings (3 min) – Effective communicator Isaac Holyoak teams up with leadership guru Toni Tsai on shape a virtual space that builds connection and purpose.
-
How Utah’s Cardiovascular Center Made (and Sustains) the Transition to Virtual Care (6 min) – Director Lora Stratton and cardiologist Anu Abraham share what team creativity and rapid problem solving looks like in practice.
Graham Walker
Jeff Elton
Erin McCormack
Nickole Canfield
Mari Ransco
With careful communication and teamwork, technical supervisor Lindsey Garcia, family medicine physicians Susan Pohl and Bernadette Kirarly, and associate director of strategic projects Erin McCormack share how Madsen Family Practice made it easier for patients to schedule virtual appointments and access the primary care they need.
Health care delivery is ripe for digital disruption. How are we preparing for the future at U of U Health? Chief Information Officer Donna Roach outlines the path forward and what it takes to transform health care to meet an increasingly digital future.
How are we building digital literacy? Chief Information Officer Donna Roach and Sr. Director of Patient Experience Mari Ransco share how using design thinking and seeing care through the eyes of our patients is a great place to start.
