What is a bundled payment?
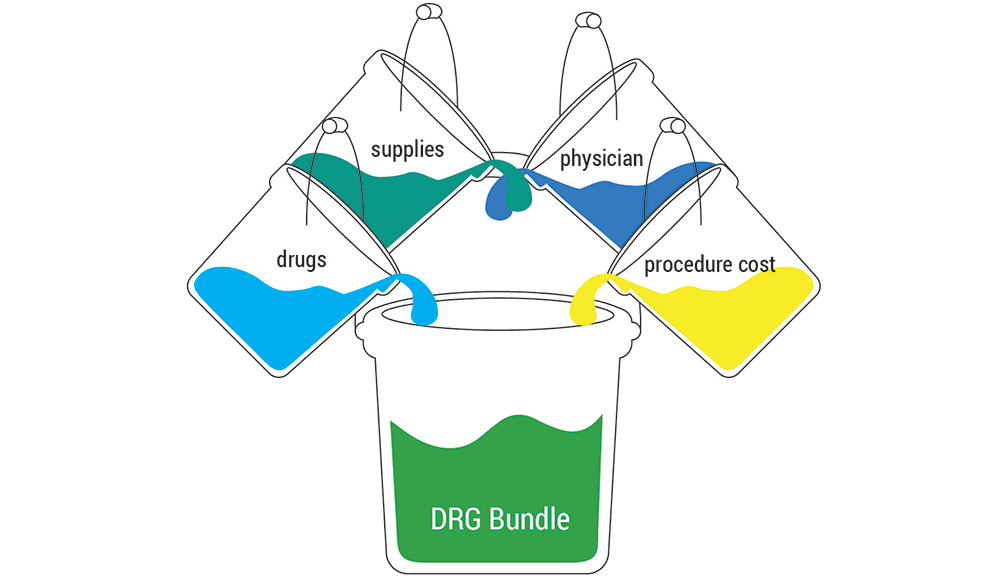
“bundle” comes in many forms. A bundle places the different components of patient care into a single bucket – a bundle – and then a set price is determined. In the rest of healthcare, this is not how payment works. In the fee-for-service structure, each interaction comes with its own price. A patient will receive a separate bill for a scan, test, or a clinic visit, even if those visits are part of one medical condition. A bundle changes that.
Bundles can be limited to inpatient care or can expand to include pre-operative care planning, outpatient services, and post-acute care. For this explanation we will focus on a bundle of inpatient care.
One patient’s inpatient stay can include anything from ten to over one thousand codes associated with surgical procedures and supplies, anesthesiologists, physician consults, etc. Each of these codes correlates with a charge.
Instead of separate charges for the individual parts, a bundle assigns one charge for the entire episode. Rather than billing for, and then receiving, separate payments from a payer for each individual component a single bill is sent to the payer and a single payment is made. This billing structure streamlines the financial aspects of getting paid for work and provides clear delineation for physicians and care teams for what is part of, or excluded from, a given bundle.
Why were bundles created?
Bundles were created to improve care for the patient, and to increase financial stability for the payer and provider organization. Patients benefit from having a team of providers focused on improving care processes, which often result in reduced procedures, supplies, and transition time. For payers, a bundle helps them pre-determine the price they will pay for care, meaning they know the exact amount they will pay for an episode of care. Care providers benefit because a bundle pays them a predictable amount, even if the costs associated with that care are under that set bundle amount (which often comes about via care process improvement).
Bundles help create stability in the healthcare marketplace. Relative to other payment model options, they are relatively easy to create, administer, and understand.
Zac Watne
What does healthcare really cost to deliver? And does the cost really make a difference in patients’ health and experience? The University of Utah tackled this problem with the creation of Value Driven Outcomes (VDO), a program to enable local clinical decision makers to lead improvements in care delivery relative to cost, quality, and service.
Instead of allowing external performance measures to define our success, we define success by reliably delivering the best possible care with empathy, coordination, and efficiency at the lowest possible cost.
When Amazon, Berkshire Hathaway, and JP Morgan Chase & Co. announced their plans to partner up and tackle “the ballooning costs of health care,” our industry underwent a collective shudder. Thankfully, Utah’s payment innovation manager Zac Watne is back to help us unravel the complexity.