Learning Objectives
1) Recognize the three forms of microaggresions
2) Describe the negative impacts of microaggressions on your learners
3) Practice willing awareness, deliberate action, and timely mitigation to confront microaggressions
Case Study
As a pediatric intern, I was on a busy critical care rotation and nervously working through my first set of nights. For weeks, I had been caring for a very sick patient, and had gotten to know the patient’s parents well. One evening, while donning PPE prior to entering his isolation room, the bedside nurse opened the door and handed me a trash can. Quickly recognizing my puzzled glance, the nurse set the bin down and, in an almost inaudible whisper, said “oh, you’re the doctor.” I made eye contact with the patient’s mother who looked a bit shocked. I didn’t think much of it; I was wholeheartedly focused on the patient. I carried on examining him, reviewed the night’s orders, and had a quick chat with his mother. Upon exiting, I said to the nurse “as for that trash can, I haven’t a clue where it goes.”
Much to my surprise, the patient remained stable through the night and I did not have any other interactions with his nurse. Eager to share such good news at morning sign-out, I told the team, “The patient had such a good night that his nurse didn’t need much from me and even thought I was an environmental service worker!” The critical care attending overheard me, swung his chair around with jaw dropped, and asked if I was okay or needed to talk. “No, why?” And in that very moment, it hit me — “Oh, because I’m Brown.” After a few nervous chuckles, the team wrapped up sign-out, and I went home to reset for the next night.
| Discussing abuse/microaggressions is and always will be difficult and sensitive. Our case study is not used to under-value any type of work. Rather, we describe a lived experience to make visible the negative impact of presuming positionality; that people of color are not often presumed to be the doctor, first. Or it could be that women of color are not often seen as the doctor, first. Marginalized people experience prejudices in different ways. What is not different is that it hurts the victim deeply, no matter their class, ability, race, gender, and/or sexuality. This case describes a common, though vastly under-recognized, occurrence. Its purpose is to signify the underlying problem that leads to prejudicial behavior, which is anchoring on "group identity" and appropriating individuals to a group based on one’s own bias before considering the individual. Unfortunately, these actions not only discriminate one individual, but also an entire group. |
icroaggressions commonly occur in medical settings creating psychologically unsafe environments of learning, working, and healing. Learners, educators, and patients can receive, inflict, or witness subtle acts of discrimination. In this article, we highlight microaggressions that are affecting our learners and call on clinician-educators to become aware, active allies or upstanders in real-time to create safer, braver spaces.
What are microaggressions?
Microaggressions are subtle, almost imperceptible, insults or indignities that communicate hostility towards a person or group’s identity, irrespective of intentionality. The hostility, verbal or non-verbal, is a an act of discrimination against one’s race, sexuality, ability, religion, gender, socioeconomic status, age, or intersections of these identities.
Words Matter
Historian, author, and anti-racist activist, Ibram X. Kendi, Ph.D., challenges the term microaggression in his book How to be an Anti-Racist.
He explains that “aggression is not as exacting a term” and commits to using the term abuse because it “accurately describes the action and its effect on people.”
The term microaggression is not novel. In his 1978 paper "An Experiment in Racism: TV Commercials," Harvard psychiatrist Chester M. Pierce, MD, coined the term microaggression to describe subtle pro-racist behaviors. The term was later popularized and thoughtfully categorized into three forms of microaggressions by Columbia University psychologist, Derald Wing Sue, Ph.D.
|
Form |
Description |
Examples |
|
|---|---|---|---|
|
Microassault |
|
|
|
| Microinsult |
|
|
|
| Microinvalidation |
|
|
Why is confronting microaggressions necessary?
Microaggressions normalize oppression and perpetuate systemic social misunderstandings of marginalized communities. In medicine, we expect our learners to thrive in their commonplace of training. It is harmful and wrong to expect that our learners will accept abuse without our acknowledgement.
Unfortunately, clinician-educators are often not aware of or do not understand the lived realities of learners. Learners suffer in silence while still figuring out how to thrive amongst their peers. They are made to feel the “otherness” of their identities, which jeopardizes their self-efficacy and resilience.
Learners experience microaggressions daily without warning. With the COVID-19 pandemic, we know more than ever that perpetual uncertainty can be distressing and cause adverse health outcomes. Victims of microaggressions can experience depression, anxiety, self-doubt, isolation, and trauma. And because microaggressions are often refuted and defended by plausible reactions, they can leave the victim feeling invalidated. Therefore, acts of omission or commission by clinician-educators — not recognizing, remaining silent, or contributing to the indignities — deepens the pain of microaggressions and contributes to the immense negative impact felt by learners.
How do clinician-educators confront microaggressions?
Clinician-educators are best positioned to be aware of their learners and their environments, however, they might feel ill-equipped or not empowered to respond.
Learning how to respond requires intention.
Here’s how:
1. Willing awareness
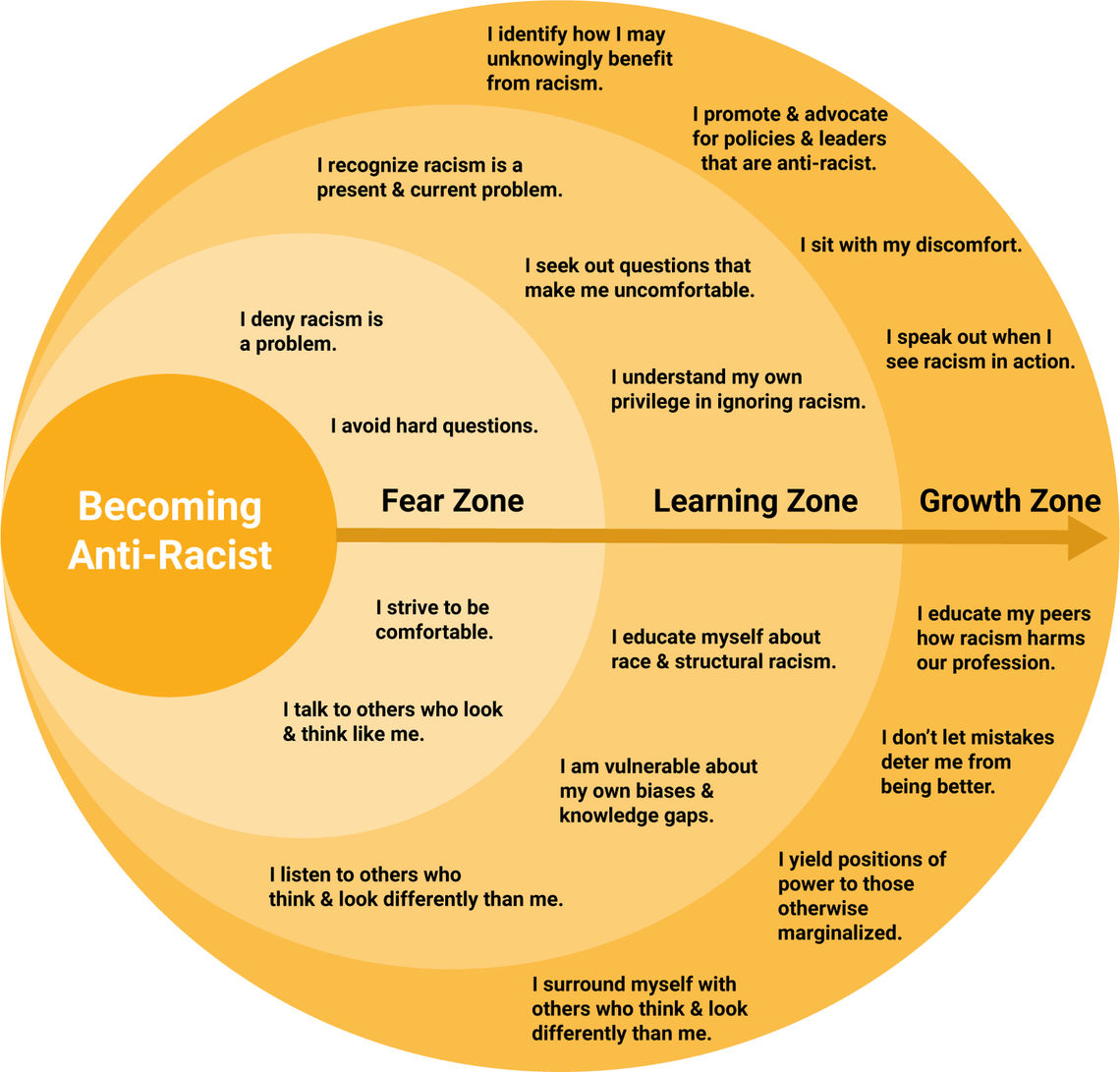
- Educate yourself. Read literature written by people with lived experiences of discrimination. Organize or participate in identity and upstander workshops at your workplace. See Local Resources below.
- Self-reflect. Take a deep dive into your identity, your privileges, your vulnerabilities, and your impact at work. Take implicit bias tests. Do it for yourself, no one else. It is a commitment to understand your narrative, question your beliefs, and ask if what you think is true. Plan to repeat the test over regular intervals. Example: Project Implicit.
- Be empathetic. You are not an imposter. You can be an ally. You can speak out for others even though you aren't like them.
- Be prepared. Before starting your week on service, take time to talk with your learners. Talk about identity and when each learner would prefer you to confront a witnessed microaggression. Some may prefer you upstanding in the moment or responding at a later time. Talk about the pros and cons of each approach together. Are there cues to look for in the moment to know how best to respond?
- Be alert. Your learners who regularly suffer microaggressions are on alert. You can be too.
When you perceive something hostile, ask yourself, would that (microaggression/abuse) happen to each of your learners? If your answer is no, then it was targeted. And your learner is hurt.
2. Deliberate action
Silence and not acknowledging what happened is NEVER the response.
- Take a deep breath
- Look at your learner, respect their cues
- If appropriate, choose to respond in the moment
- Look at the perpetrator
|
Pause the conversation. [clear your throat or hold up your hand] |
“Excuse me, before you/we continue, I’d like to speak up.” “Could I interrupt for a moment?” “Before you/we go on, I’d like to acknowledge what just happened.” |
|
Name the behavior as inappropriate and set boundaries. |
“What you said/did to my learner___ made me feel [emotion, e.g. uncomfortable].” “We don’t use that language here.” “Let’s keep it professional.” |
| Seek clarification. |
“What did you mean when you said/did ___?” “I'm worried that your comment/gesture hurt/dismissed my learner, what do you think?” “I’d like to understand your perspective. Is there something that affected you that prompted your reaction?” |
|
Value your learner. Validate their worth on the team. |
“I respect every member on my team. I expect that you do as well.” “___ is one of my learners. I do not appreciate anyone treating my learner this way.” “[I agree with ____,] what happened was not appropriate or deserved, no matter how benign it seemed.” |
| Refocus the discussion to the professional context. |
“You may have been trying to compliment/joke, but let’s get back to why we are here/what we are here for.” “I know this is uncomfortable for everyone, but it needs to be acknowledged so we can all create safe, brave spaces to speak up.” “I am willing to come back and discuss this further with you, but for now let’s focus on____.” |
- If the learner responds first, don’t overshadow their agency, but don’t move on. Stay engaged and provide support if needed.
- At any point, if you are worried that confronting or continuing the conversation will bring more risk to the learner or it is not their preference for you to speak up, it is ok to acknowledge the interaction later with timely mitigation.
3. Timely mitigation
Do this step, ALWAYS, even if action wasn’t taken.
- Place the responsibility on yourself. This prevents your learner from suppressing the abuse.
- Ask the learner to debrief soon after or at a later time.
- Prioritize and make a dedicated time.
- Find a quiet, safe space. In-person is preferred, though due to the pandemic, video or phone call can be an option.
- Acknowledge the interaction, use "I" statements, be curious, name the feeling/emotion, be ready to validate, and offer supportive action.
- Don’t make the conversation about you. Let the learner(s) take the lead.
The best practice is to practice. You will know that you’re doing it right when it starts to feel more right to you. When you get it wrong (and you will), lean in, make an effort, and repair that interaction by challenging your own resilience. Model your vulnerabilities.
Conclusion
Let’s return to the case study. The pediatric intern experienced a racist abuse, a microinsult based on the color of her skin. Upon first interaction, she was quickly mistaken to be the environmental service worker, not the doctor. It was an unconscious, subtle gesture that assumed her identity. The response from the nurse and mother was silence. After the attending heard about the microaggression, it was supportive to ask if she was ok and wanted to talk, but she was post-call. She was left with uncertainty of whether anything would be done and whether her attending would reach out again. Throughout residency there was no closure for her.
Here’s what the clinician-educator could have done to confront the microaggression:
| Willing awareness | Be prepared, what would your resident want you to do? |
| Deliberate action |
Find an appropriate time to validate the learner:
Find an appropriate time talk with the nurse:
|
| Timely mitigation |
“Do you mind if we find a good time to debrief about the microaggression from earlier?” “What happened was not fair. How are you doing?” “How did you feel it was handled in the moment?” “What can I do to support you?” “I want to foster an inlcusive environment. Next time this happens, I commit to speaking up faster/reaching out sooner.” |
Resources
- Pierce CM, Carew JV, Pierce-Gonzalez D, Wills D. An Experiment in Racism: TV Commercials. Education and Urban Society. 1977;10(1):61-87. doi:10.1177/001312457701000105
- Sue DW, Capodilupo CM, Torino GC, et al. Racial microaggressions in everyday life: Implications for clinical practice. American Psychologist. 2007;62(4):271-286. doi:10.1037/0003-066X.62.4.271
- Young K, Punnett A, Suleman S. “A Little Hurts a Lot: Exploring the Impact of Microaggressions in Pediatric Medical Education.” Pediatrics. 2020;146(1):e20201636
- Shankar M, Albert T, Yee N, Overland M. Approaches for Residents to Address Problematic Patient Behavior: Before, During, and After the Clinical Encounter. Journal of Graduate Medical Education. 2019;11(4):371-374. doi:10.4300/JGME-D-19-00075.1
- Molina MF, Landry AI, Chary AN, Burnett-Bowie S-AM. Addressing the Elephant in the Room: Microaggressions in Medicine. Annals of Emergency Medicine. Published online May 2020:S0196064420302596. doi:10.1016/j.annemergmed.2020.04.009
- UU Resiliency Center is holding virtual group sessions for providers and staff who are Black, Indigenous and people of color (BIPOC) to share stories and find safe places to mitigate silent suffering. Sessions will be facilitated by Trinh Mai, LCSW and held every Thursday at 12:30 PM via Zoom. BIPOC Check-in & Support For more information please email: Trinh.Mai@utah.edu
- UU GME Wellness Program is providing inclusive workshops during GME orientation, retreats, or any blocked protected-time to discuss identity and role play scenarios using the Identity and Impact toolkit and Stop, Talk, Roll workshop. To set up a workshop please email our GME Wellness Champion: Katie.Gradick@hsc.utah.edu
- UUH Accelerate: Connect Leadership has an archived webinar by Amy Cowan, MD on White Identity: Race and Racism June 11, 2020.
Perspectives pieces
- Montenegro RE. My Name Is Not “Interpreter.” JAMA. 2016;315(19):2071. doi:10.1001/jama.2016.1249
- Unaka NI, Reynolds KL. Truth in Tension: Reflections on Racism in Medicine. J Hosp Med. 2020;(2020-06-25 ONLINE FIRST). doi:10.12788/jhm.3492
- Cowan AN. Inappropriate Behavior by Patients and Their Families—Call It Out. JAMA Intern Med. 2018;178(11):1441. doi:10.1001/jamainternmed.2018.4348
Books on racial identity and microaggressions
- Oluo, I. “So You Want to Talk About Race.”: United States: Basic Books. 2019.
- Tatum BD. “Why Are All the Black Kids Sitting Together in the Cafeteria?”: And Other Conversations about Race. Basic Books; 2003.
Toolkits and workshop resources
- Sandoval RS, Afolabi T, Said J, Dunleavy S, Chatterjee A, Ölveczky D. Building a Tool Kit for Medical and Dental Students: Addressing Microaggressions and Discrimination on the Wards. MedEdPORTAL. 2020;16(1):mep_2374-8265.10893. doi:10.15766/mep_2374-8265.10893. https://www.mededportal.org/doi/10.15766/mep_2374-8265.10893
- Stop, Talk, Roll. Georgetown University School of Medicine website. https://som.georgetown.edu/diversityandinclusion/studentorganizations/stoptalkroll/
- Primary Care Progress: Identity and Impact Relational Leadership Toolkit. https://www.primarycareprogress.org/wp-content/uploads/2020/06/Toolkit-Identity_RRI.pdf
*Originally published in April, 2020
Reena Tam
Margie Diaz-Ochu
The crises of Covid-19 and police brutality have highlighted systemic racial inequity in the United States and the need to consciously dismantle the forces that cause racial health disparities. PA students Scarlett Reyes and Jocelyn Cortez brought together Black patients at the University of Utah to share their experiences. Their advice: build cultural competence and be mindful of microaggressions.
With so much going on around the world and in our daily lives, our brains are constantly in overdrive. Mindfulness educator and social worker Trinh Mai explores what practitioners across U of U Health and the VA are doing to help their patients and teammates take a mental break and respond courageously in these times.
Michael Danielson, organizational development consultant, shares a personal experience about privilege, respect, and friendship. When his comfortable cultural norms failed him and led to a regrettable interaction, he learned that respect is demonstrated by taking action, and that you have to step out of your comfort zone to change culture.