Quick Language Guide
Click here for a guide to inclusive language developed by Christina Necessary, Jacob Knight, Raquel Maynez, Bridget Dorsey, Jessica Kunzman, Chieko Hoki, and Tiffany Ho.
University of Utah School of Medicine students, we are learning how to provide compassionate patient care. We are working to offer personalized care that meets each patient where they are and addresses their needs.
As we attended class, both in lectures and in clinical settings, we noticed one area of patient care where we didn’t have the resources to provide personalized care: inclusive language.
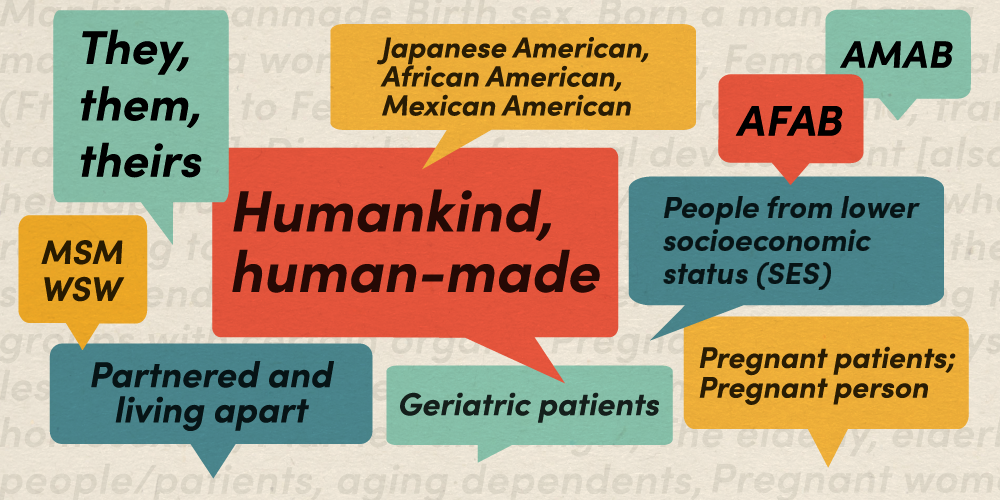
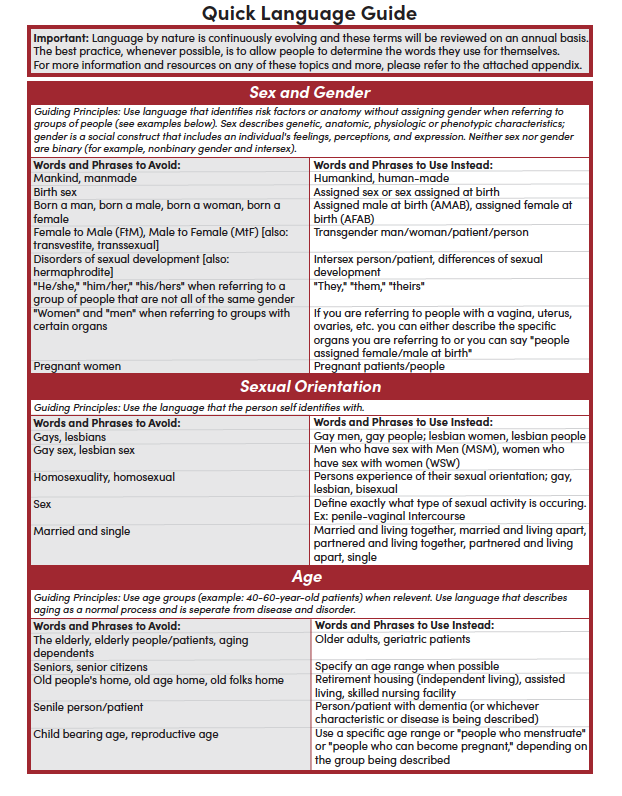
We came together to develop the Quick Language Guide. This reference sheet for students, providers, and lecturers helps ensure appropriate language use when it comes to topics including:
-
Sex and gender
-
Sexual orientation
-
Age
-
Race and ethnicity
-
Socioeconomic status
-
Health identities
This sheet also includes links to more extensive language guides as well as articles that focus on incorporating equity and inclusivity into medical practice, teaching and research.
Incorporating inclusive language into medical education
The language guide shouldn’t be viewed as just a reference, but as a jumping-off point for lessons and education. We use the guide in the transition to medical school week as an activity for first year and second year students. We ask what phrases they avoid using and what they recommend using instead.
During these brainstorming sessions, we can draw students’ attention to inclusive language. We can open their eyes to types of language they may not have thought of before, beyond pronouns and race. This activity can set a foundation for using inclusive language in school and clinical settings throughout their career.
The importance of inclusive language in healthcare settings
Medicine is about more than just medical knowledge; it’s about developing a trusting relationship with patients. To build this relationship you must demonstrate respect and earn trust from your patients. Language is one way to do that.
Using inclusive language can help patients feel comfortable, accepted and safe. It’s a way to start a connection by respecting who the patient is.
Language also affects how we think about patients and how we care for them. It is part of our foundation for how we see the world. Using inclusive language can help us identify our implicit biases and reduce stigmas around different health conditions. It can help us improve how we approach people who might not look like us or have the same background as us. This is truly the basis for providing higher quality, more compassionate care.
How medical providers can use inclusive language
The first step to using inclusive language is to reflect on our own language. We should ask ourselves questions such as:
-
What terms do I often use?
-
Why do I use these terms?
-
What is the response of others to the terms I use?
-
Am I using the most appropriate term?
-
What terms can I use instead?
For instance, we often get questions such as what should I say instead of “mother” or “pregnant woman” to be more inclusive? By taking time to reflect on this yourself, you can often find the answer for yourself. What is it that’s most important in that situation? Typically, the answer is that the person is pregnant or that the person has a uterus.
By reflecting on ourselves, we can develop the skills to address new issues that arise in the future. No language guide can answer every question people might have. So being able to think critically about language on your own will help you address the new and unique situations you find yourself in.
When in doubt, healthcare providers should ask the patient what terms they prefer for themselves and their bodies. Patients might not care to be called a “person with diabetes” but prefer to just be called “diabetic.” We can match our language to meet each patient’s preferences and make notes in their charts about what language meets their needs.
Inclusive language is always changing. While this language guide is a helpful tool, it is not the be-all or end-all for being inclusive in our practices. To improve the quality of our patient relationships, we encourage healthcare providers to use this guide and expand on it in their own practice.
We encourage you to adopt a growth mindset and to be open to learning more about yourself and your patients, so we can provide the best care possible.
Christina Necessary
Jacob Knight
Raquel Maynez
Bridget Dorsey
Jessica Kunzman
Chieko Hoki
Tiffany Ho
In an era where equity, diversity, and inclusion (EDI) are paramount for organizations striving for meaningful change, the challenges of prioritizing and advancing EDI initiatives have come to the forefront. Experienced EDI professionals William Smith and Katty Youd share valuable insights on the challenges and strategies involved in advancing EDI initiatives, from fostering trust and facilitating conversations to navigating cultural shifts and institutional support.
We often overlook the wealth of diverse cultural experiences and perspectives that profoundly influence the well-being of our students and patients. Educators Kerri Shaffer and Nina Feng leverage community cultural wealth to transform healthcare education for a more inclusive future.
Free clinics serve as a vital pillar for urgent medical care for underserved populations in our community. Four Physician Assistant students at University of Utah explain how their involvement in student-led free clinics have benefited the community—and their medical education.