Teamwork Must-Have: Compelling Vision

We’ve distilled the wisdom of our system’s best change agents into 15 success factors for vision.
eaming is one of those words that doesn’t make sense to me right away (with all due respect to Amy Edmondson). What teaming means to me is creating a learning environment where you can make mistakes, pick yourself back up and keep trying to get better. It’s the ability for a group of people to tackle a problem together in a safe-to-fail environment.
When I became the system’s nursing director of capacity management, we had to create a system out of disparate parts. In 2012, individual nursing units made decisions that best served their needs and discharges felt rocky and unplanned to patients and care teams. Patients frequently told us that it took hours to actually leave the hospital after being told they were going home. Because many of our patients come from far away, we were often sending recently-discharged patients and their families out with long, late drives ahead of them.
It was a huge (and ongoing) change. To really fix this problem, it had to be okay to try things and keep learning. We wondered–what if each unit could develop and knew the plan for managing their beds every day? What if we could understand our system’s capacity in real time? What if we could exceed patient expectations?
Our vision was to get every single patient in the right bed at the right time. It was an audacious statement at the time. Nobody had tackled this system-level problem. My team and I realized that hundreds of people impact how patients move through our hospital, so we asked “How do we influence and bring all these people together, to adopt this vision and help improve this process for our patients?”
1. Culture change
When we started to talk about improving discharges, there was a lot of skepticism. “We’ve worked on discharges before and it didn’t work” or “here we go again.” We embarked on a campaign to change our mindset from being victims of our capacity and helpless to do anything, to owning our capacity and empowering everyone to have an active and engaged role in improving it. We created a culture of don’t be afraid to try: you never know, it just might work.
2. Plan for the day and plan for the stay
The Daily Unit Huddle is a predictive model of managing day of unit capacity and demand, and unit level problem solving for mismatches. Standardized, unit based interdisciplinary discharge meeting that looks at all patients identifying goals, barriers, and target dates. Tiered daily huddles bring issues in real-time to the system level with solutions back to the local level.
3. Interdisciplinary hospital capacity meeting
Led by the clinical nursing supervisor this team includes charge nurses, environmental services, transport, and security, they develop a system level plan for how we will manage the day. Identifying pressure points, priorities, barriers, and what resources are needed to be successful in meeting our vision of the right patient, in the right bed, at the right time. We talk about ALL of our patient’s needs.
Results
The results of our efforts have been inspiring. Patients are getting out of the hospital earlier, despite the fact that we have increased the number of monthly discharges by 35% since 2015. Patients are noticing. Our HCAHPS Discharge Information has improved.
Improved Patient Experience:
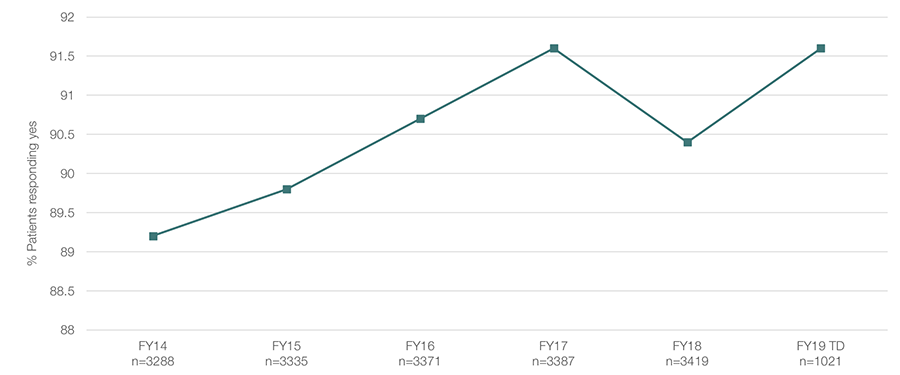
HCAHPS; Percent responding yes.
What I learned
Here’s two ingredients to creating a learning environment during change:
The Power of the Interdisciplinary Team
Everyone has input that matters. Even though my work is at a system-level–our hospital’s inpatient bed capacity–I have to work proactively to build bridges with others. It’s easy to work in isolation and focus on our own individual problems. We’re an organization filled with incredibly passionate people who want to go and fix problems right now because it’s the right thing to do for the patient. But fixing things in one area can break process for others. You think you’re doing the right thing for one thing, but it leads to problems for others.
You do have time
It can be challenging to get everyone together as you start to look at hard, complex problems. It can take weeks, if not longer, to pull a meeting together with all the people who are touched or involved in that problem. But if you don't take the time to bring everybody together to understand the depth and the scope of your problem, it's going to take you ten times longer to get it solved. You’ll break it along the way, and you’ll have to go back to the beginning. You do have the time. Use it to get people together and you'll be far more successful.
We’ve had an amazing team of leaders who work tirelessly for our patients and our system.
Annotated transcript from Tracey Nixon's presentation at the Oct. 31, 2018, Leader Development Institute in Salt Lake City, Utah.
Thank you to the team:
Greg Boseman, Mason Milligan, Stephanie Stapleton, Rasa Butkus, Jane Nielsen, Spencer Steinbach, Susan Clark, Chris Noren, Shegi Thomas, Andrew Davies, Melinda Patterson, Steven Thordensen, Anne-Michelle Ferko, Cooper Riley, Jane Wall, Shirleen Gamonal, Sonya Ruelle, Andrew Wood, Jared Lofgren, Derrick Shepherd, Lawrence Marsco, and Chris Shirley.
Tracey Nixon
Depression is one of those problems so big and so pervasive that tackling it seems impossible. That's why process improvement is so powerful: by setting one goal—improving depression screening rates—11 U of U Health Community Clinics are making the impossible manageable.
Biometric identification is a national best practice — but adapting that to a local environment isn’t easy. Although it’s rare, confusing an identity can have scary consequences (like getting a prescription for a drug you’re allergic to.) So Doug Ostler and his team worked to implement palm scanners and make patients feel safer.
The hard work of improving value includes leading and engaging a team. Two improvers, Emily Carlson and Dr. Lauren Wood, share how they kept their teams engaged throughout a long (and sometimes inconclusive) improvement process.