aiting is such a firmly entrenched feature of health care that it is often expected–notice the large comfortable waiting rooms included in every hospital and clinic building. Waiting is not recognized for the disrespect it conveys. Wait time sends an unambiguous and often unintended message that the physician considers their time more valuable than the patient’s. The solution starts with the right team.
Patients describe Dr. Robert Tashjian as an incredible communicator, teacher, and skilled shoulder surgeon. But two years ago, they also described the legendary wait time to see him. Several changes in Tashjian’s team and culture have made a difference. Now, when patients wait, it’s not nearly as long or as frequent.
Voice of the patient – Before improvement
"I LOVE Dr. Tashjian and feel he is probably the best shoulder surgeon in the state. However, I would not feel comfortable recommending to others. Had I known it was going to be almost 90 minutes to see the Dr. I would have rescheduled. My time seems to have little importance, while I respect that of a very busy doctor." (Press Ganey survey data, visit: 12/2014)
"I LOVE Dr. Tashjian and feel he is probably the best shoulder surgeon in the state. However, I would not feel comfortable recommending to others. Had I known it was going to be almost 90 minutes to see the Dr. I would have rescheduled. My time seems to have little importance, while I respect that of a very busy doctor." (Press Ganey survey data, visit: 12/2014)
Voice of the patient – After improvement
"This clinic is so well-run. Please teach everyone how to do this! Thank you so much for having a few nights with late afternoon and evening hours, as well as a few Saturdays. This has helped me so much!" (Press Ganey survey data, visit: 04/2018)
"The wait time has markedly lessened since I was Dr. Tashijan's patient in 2016. I really appreciate that, as I often dreaded my post op appointments unless I was seen first thing in the morning." (Press Ganey survey data, visit: 03/2018)
The Science of Scheduling
Sound complicated? Don’t go it alone. U of U Health has a dedicated team who specializes in streamlining clinic schedules. Learn more.
The team frames the physician: Ian Crossett
Dr. Tashjian’s practice is busy–we see 25-40 patients per day in clinic. When I first started at the University Orthopaedic Center two years ago, I had to learn the current process. Sometimes patients would wait over an hour in the waiting room or in the clinic to see Dr. Tashjian. It frustrated everyone–patients, medical assistants, residents, front desk check-in, and of course, Dr. Tashjian.
I realized–if you save a minute per patient and multiply that by 40 patients per day, you’re saving 40 minutes. We started small by making minor changes to the template. The template determines the flow of the day and the number of patients we’ll eventually have in the operating room.
Four things you can do to get started
1. Analyze your current data
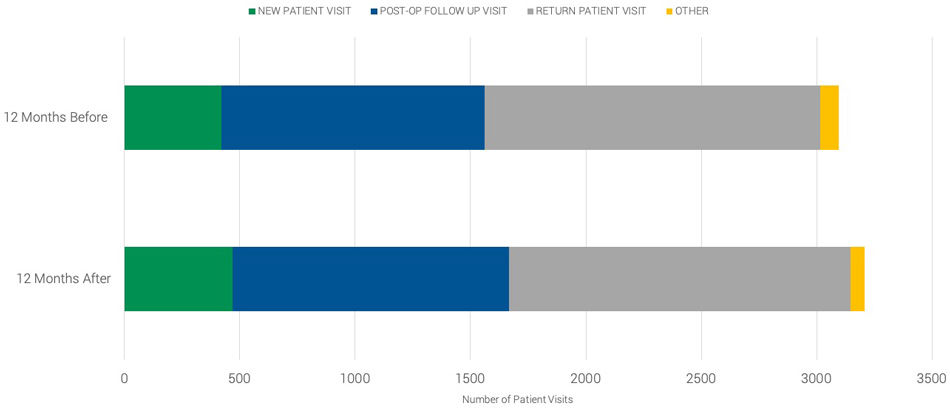
We discovered through analysis and anecdotes that we were often scheduling unplanned return patients into slots for new patients. This reduces the number of available appointments for new patients, sometimes pushing out a new patient visit by weeks. We know patients wanted more access, and we did too.
2. Define each visit type and the length of time it requires
We looked critically at the visit type and time. How many return visits does each operation require? Dr. Tashjian prefers to see post-operative patients five times: at two weeks, six weeks, 12 weeks, six months, and one year after the procedure. Beyond the first post-operative visit, those visits weren’t scheduled or planned for in his template. We changed the template to include five return patient slots per operative case based on the average number of cases Dr. Tashjian performed over the past three years. This ended up creating a template with a new patient to return patient ratio of approximately 1:2, which seems to be the sweet spot.
We also looked at when we were scheduling appointments. If we know we want to see a patient five times, let’s schedule those five appointments on the day of surgery instead of waiting and squeezing them in.
3. Plan a mix of visits for each day
Dr. Tashjian’s clinic used to squeeze people in, which makes an individual patient feel that their needs were responded to. But every time you squeeze in some patients, you’re squeezing out other patients. We tried to minimize that by making our template reflect exactly what we needed.
We now space return visits slots evenly throughout the day with dedicated new patient slots, allowing our team to catch up from any delays and eliminating the need to double book standard follow-up visits. We also freeze some new patient slots until seven days prior to the day of clinic, when they automatically change to return visit if not filled.
4. Add (some) time to increase access
In addition, we’ve added one half-day Saturday clinic per month, occasionally two half-days per month. Those appointment slots open only two weeks prior to the day of clinic, which allows for urgent new patients or unexpected return patients to be added. These changes reduced the need to absorb unanticipated return visits during the week.
Improving team culture
Falling behind is the exception, not the norm. There are less patients in the waiting room. Our team feels happier and looser. Dr. Tashjian now has the time to personally connect with our team during clinic – joking, asking about weekend plans. Our staff is less stressed. I’m sure patients can feel that. When you get the template right, you can spend time doing things you really want to do: connecting with patients and making sure their care is just right.
The results
Improved patient experience and decreased wait time
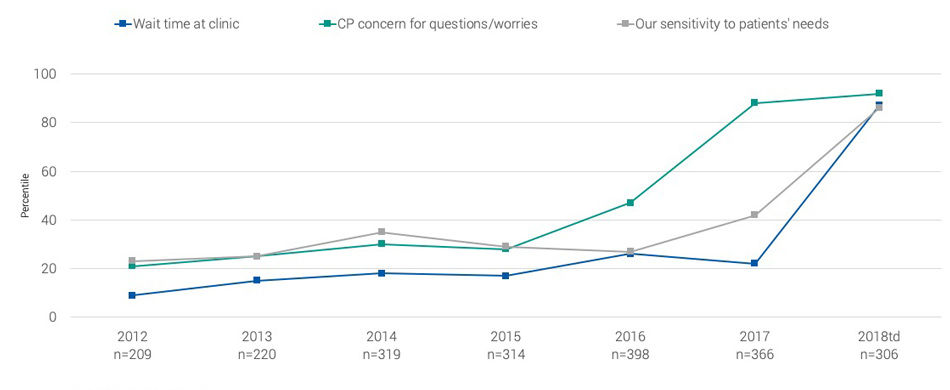
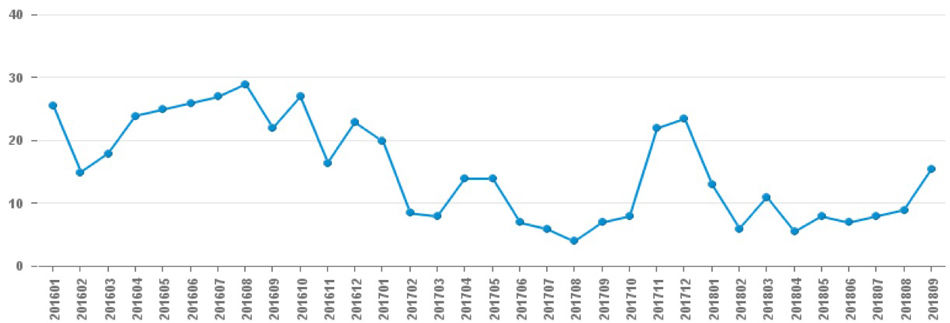
Improved new patient access
Improved scheduling: Now seeing more new patients
 The physician's perspective:
The physician's perspective:
"We have the right team."—Robert Tashjian, MD
I have tried many things to reduce wait times in past years. We tried multiple iterations: a whiteboard set up in the back of clinic with every patient and their time in/time out listed. Stopwatches hanging on the doors, with medical assistants (MAs) knocking if an alarm went off and I was in a room for too long. Despite all of that, we couldn’t figure out how to make the system work based on the 38-40 patients we see throughout the day.
Ian was a tremendous help. As a provider, I had to give Ian the autonomy and the trust to make decisions to improve our system.
What Ian did was significant: He makes sure our clinic flow is correct, looking ahead to position patients who might be more challenging in the right place. If we spend extra time in clinic with tricky patients, but their appointments fall before lunch or at the end of day, we don’t fall behind. The difference is we get done at 5:00 PM instead of 7:00 PM—and it actually feels like we do more work.
Third, we have the right team. It’s about having the right mix of people to make the system work. We have two MAs who are incredible. We used to have a system where specific MAs performed specific responsibilities. Now, everyone is trained to do everything. If someone is running behind, someone else on the team can pick up the slack. Anyone can room a patient or make a phone call. Everyone on the team has independent, interchangeable, cross-trained skills. I’m the only one who can’t do everything.
Ian Crossett
Robert Tashjian
When dermatologist Dr. Stephanie Klein proposed a clinic for urgent skin care needs, she thought it would be easy. Reserve the clinic rooms, schedule the appointments—done! She quickly found out that moving from idea to reality would require leadership skills that she hadn’t been taught in medical training and ten years of practice. Accelerate’s Mari Ransco found out how Klein transformed from busy clinician to leader.
If in previous dojo posts, you still haven’t found what you’re looking for, today’s post will satisfy your desire. In it we describe the mysterious ways of Drs. Chris Hull’s and Mark Eliason’s clinic practice. Unless you’re a patient, you can’t witness their clinic, but this post is even better than the real thing.
Waiting is such a firmly entrenched feature of healthcare that it is often taken as a given and not recognized for the disrespect it conveys.
