How UNI’s HOME Program Changed Its Culture
he HOME Program’s medical director of primary care, Dr. Kyle Bradford Jones, and former director Dean Weedon shared their lessons learned in their recent New England Journal of Medicine NEJM Catalyst article. Accelerate’s Mari Ransco interviewed Dr. Jones to learn how the HOME program has truly integrated care.
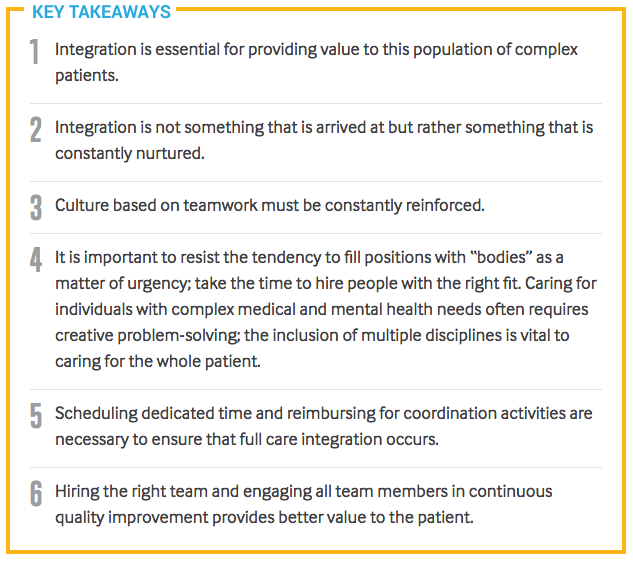
“Integration, or the active coordination of behavior and decision-making across clinical disciplines and providers, is a buzzword in health care and is more of a continuum than a singular action. Integration involves more than simply co-locating team members and services,” wrote Dr. Kyle Bradford Jones and Dean Weedon in the recent article.
UNI’s 4 Lessons for How to Integrate Care:
1. Incorporate (and compensate for) time for care integration
In addition to having a shared workspace, daily meetings, workflow, and compensation are all structured to reinforce integration. Providers at the HOME program are paid a salary that accounts for care coordination as part of each provider’s productivity expectation.
2. Reduce perceived power differentials by creating meaningful provider partnerships
Physicians are partnered with advanced practice clinicians (APC), such as a nurse practitioner. The providers work together to share the workload and coordinate as a team. The goal is shared responsibility for patient care and outcomes, not rank-and-file supervision.
3. Design a new role to enable team integration and care coordination
HOME developed the case analyst role to coordinate care between the patient’s family, extended care team, and community agencies. These individuals are hired based on experience with this patient population, rather than previous medical training.
4. Hire on the basis of passion and collaboration
Culture means hiring the right people to do the work. The HOME program hires highly competent, collaborative individuals with a track record of commitment to their work. Leadership embraces a flat hierarchy, giving every team member a voice to contribute to the broader mission of improving patient care.
Where to Start?
The authors outline three recommendations to begin integration in your care setting:
- Promote predictable access to team members and dedicated time for coordination and communication.
- Hire to support the culture, and cull those who do not fit the culture.
- Invest in a role to enable coordination, such as the case analyst.
When asked how the HOME program’s structure has influenced his practice, Dr. Jones replied, “This wasn’t always my plan, but I’ve really come to appreciate having more team members to rely on and the ability to coordinate with people immediately. It’s better for us and the patients.”
Share and Spread the Work
As a nationally recognized academic health system, University of Utah Health faculty and staff contribute to the spread of innovation by sharing great work both inside and outside of the organization. By publishing this effort in NEJM Catalyst, Dr. Jones and Dean Weedon’s team are sharing and spreading best practices to improve health care.
We commend their efforts and look forward to learning more from them (and you) in the future.
Accelerate Editorial Team
Sterile Processing runs a lean operation, delivering millions of instruments to University of Utah Health’s procedural teams. Director of value engineering Steve Johnson, assisted by the video wizardry of Charlie Ehlert, sheds light on our system’s unseen infection prevention heroes.
To celebrate the New Year, Value Engineer Mitch Cannon applied statistics to weight loss. He was quickly reminded of an important lesson that applies in health care: when you’re trying to improve, don’t overreact to data.
Balancing uncertainty, fear, and emotions isn’t easy — especially in health care. Family practice physician Kyle Bradford Jones looks outside of his practice to identify two common biases that affect how we behave in the face of perceived risk. His key insight? The risk that isn’t directly in front of us may be mistaken for no risk at all.