niversity of Utah Health is the only place I’ve worked as a nurse. I have 11 years of experience in intensive care units. For four years, I split my time between SICU and NCC. Six years ago, I became NCC’s nurse educator; four years ago, I became nurse manager.
The team on NCC—nurses, health care assistants, nurse practitioners, social workers, therapists, pharmacists, neurosurgeons, neurologists, neurointensivists, and fellows—is responsible for caring for critically ill or injured patients. They usually come straight from the emergency department or bypass ED altogether if they’re flown in with head trauma.
In March 2014, NCC nearly doubled, from 15 to 23 beds, becoming the largest and most technologically advanced neuro critical care unit in the Mountain West. I had to hire 20 new nurses, and most didn’t have the necessary skills for such a high-acuity setting.
This problem isn’t unique to NCC; each unit has specific patient needs that require nurses to build their practice. U of U Health has tackled this problem through a variety of supportive programs. I researched other ICUs at large hospitals to see how they dealt with it. Most had two charge nurses instead of one. I realized I had to take a new approach and build a new role that empowers nurses with some experience to support new nurses coming in.
The Axon/Dendrite role: Mentor-leader
In 2014, I created the “Axon/Dendrite,” or assistant charge nurse, role. Axon and Dendrite are the communicators of the brain cell, so it made sense for NCC. Four years after starting the program, I’ve found that the extra support produces many positive effects.
The Axon/Dendrite nurses have contributed to improved quality. We had zero central line infections in the last year. We’ve also cultivated a stronger sense of community on the unit. It’s helped me with retention, too, since our nurses report increased job satisfaction and employee engagement. I recruit new nurses by telling them that the Axon/Dendrite program serves as a first step into nursing leadership.
What does the Axon/Dendrite do?
The unit is split in half—one Axon and one Dendrite for each shift. Each assistant charge nurse takes care of one stable patient, then rounds on their half of the unit with a detailed checklist for each patient that documents chart checks, safety equipment use, physician’s orders, heart rhythm strips, intravenous lines, and utilization reviews.
The Detailed Axon/Dendrite Checklist
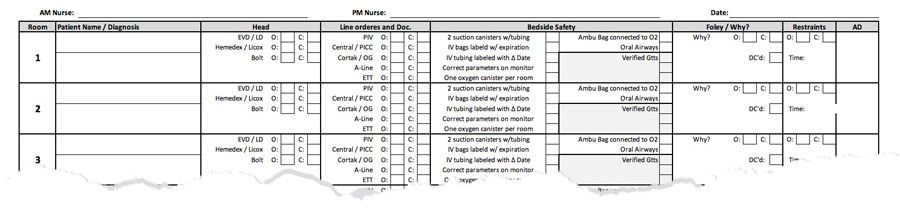
Want to adapt it for your unit? Click here to download an Excel copy.
These checklists empower the Axon/Dendrite nurses to make decisions and lead teams so they can move forward with their careers without leaving the unit. They also satisfy U of U Health’s system goals: improved patient experience, increased safety and quality, and better labor efficiency.
How (and why) it works
The expert is the person doing the work—so we asked clinical nurse Irina Choi to share her experience as an Axon/Dendrite.

Irina Choi, RN, on being an Axon/Dendrite.
Supporting the team builds trust
Helping co-workers is my favorite part of the Axon/Dendrite program. I can make the unit run smoothly—and make the work day easier for my colleagues. Sometimes it’s as simple as giving a nurse a lunch break while I do a bath with a health care assistant. When a nurse comes back and sees that, they say, “Whoa—thank you so much!” Or I can do their rhythm strips (a time-consuming process required for each patient). All of that work impacts safety, quality, and patient experience.
It’s great for our team. There’s an extra set of eyes on everything—multiple layers of safety checks. That’s especially important if you’ve got a new nurse just off orientation who is inexperienced with hospital care. It also makes the family of a patient feel like their loved one is receiving better care.
We have more time to connect with patients and families
Often, our patients on NCC aren’t able to speak, so I spend a lot of time with their families. I love that I get to be there for the family as well as the patient. I love the challenge of building trust with families. Once they trust me, they can relax. Families need to know that their loved one is going to be taken care of as a human, not just as a patient.
As nurses, sometimes we don’t think about that. We’re very focused on delivering the best quality and keeping patients safe. For patients and their families, we have to show them that we remember they’re human beings—a person outside of the hospital. Simple things like brushing the patient’s teeth might be a big deal. When family members see a nurse paying attention to their loved one, they start to trust us.
I am a mentor-leader for new nurses
Some days, my focus is with one new nurse in one patient’s room. I can ask, “What do you need help with?” New nurses have told me, “I couldn’t have done today without you. I’m so glad you’re here.” That’s huge.
The Axon/Dendrite program allows them to focus on learning and doing their job while knowing that somebody else is watching out for them and their patient’s safety. Like Emily told me when I started, “You’re not going to be alone.” She also told me right from the beginning that I had a chance to grow to that next stepping stone in my career.
Being an Axon/Dendrite highlights the fact that this hospital has your back and wants you to succeed. We’re thinking outside of the box, which helps me realize that I have opportunities to grow. I don’t have to go straight from being a clinical nurse to a charge nurse.
Being a nurse is powerful—and we’re empowering new nurses.
Nurses are there for people in some of the most vulnerable times of their lives. That’s a great privilege and a huge honor. My mother was a nurse in Russia, and she's shared lots of amazing stories. I've gone on a few different humanitarian trips around the world and realized nursing is something you can use anywhere you go. It’s a language that everyone speaks.
The Axon/Dendrite program helps new nurses grow into this profession in a positive way—and it's helping me grow as a leader in this organization.
Emily Baarz
We all make lots of mistakes early on in our careers. Hospitalist and mentorship expert Valerie Vaughn sets us up for success by sharing her expertise on how to take control of your long-term career path.
Being new is hard. Often for new faculty, it means adjusting to a new state, new team, new patients, and a new organizational culture. We asked hospitalists Ryan Murphy and Valerie Vaughn and surgeon Ellen Morrow for tips that only come from a little time under the belt.
Senior Nursing Director Rita Aguilar shares how a pivotal medical experience at the age of 17 sparked her interest in becoming a nurse. Years later, Rita is applying the same level of compassion and support she received from that experience to encourage others in seeking a career in health care and diversifying the medical field.
