The Challenge
ealthcare is full of problems that everyone has tried to fix and failed. Solutions are generated, implementations are attempted, but the results just don’t come. What if the answer isn’t generating creative solutions, but spending more time understanding the problem? Wait time in the clinic is just such a problem.
Wait time is complicated—fix one issue and another complication arises. It’s even more overwhelming when analyzing an operation as diverse and productive as the Moran Eye Center. Moran is home clinic to 35 ophthalmologists and optometrists, seeing 56,000 patients a year. Waits at Moran had always been a problem, but the patients were growing increasingly impatient.
Introduction: 17 patients at once
Maybe you’ve been in a situation similar to John Darden, Moran’s manager. One spring day, the lead ophthalmic tech rushed into Darden’s office, needing a key to the closet where the Moran Eye Center staff kept the “suck-up snacks.” She told him that it was a bad day—17 patients were all scheduled at 1:00 pm for the same provider. Darden and Collette Marthia, the Eye Center’s supervisor, sprang into action. They joined the busy waiting area to discuss the delay with patients. When the dust settled, they looked around. Some patients had waited as long as 90 minutes. How did this happen?
Listening to the voice of the patient
"The staff were excellent, but others waiting mentioned that the long wait is typical. Therefore, it seems the long wait was not for an emergency but a result of not enough staffing or over-booking of patients. The long wait time undermines confidence. Moran is 'world famous', but the office practice is not in that league. The long, long delay sends a negative message."—Visit Sept. 4, 2014
"The staff were excellent, but others waiting mentioned that the long wait is typical. Therefore, it seems the long wait was not for an emergency but a result of not enough staffing or over-booking of patients. The long wait time undermines confidence. Moran is 'world famous', but the office practice is not in that league. The long, long delay sends a negative message."—Visit Sept. 4, 2014
The Goal
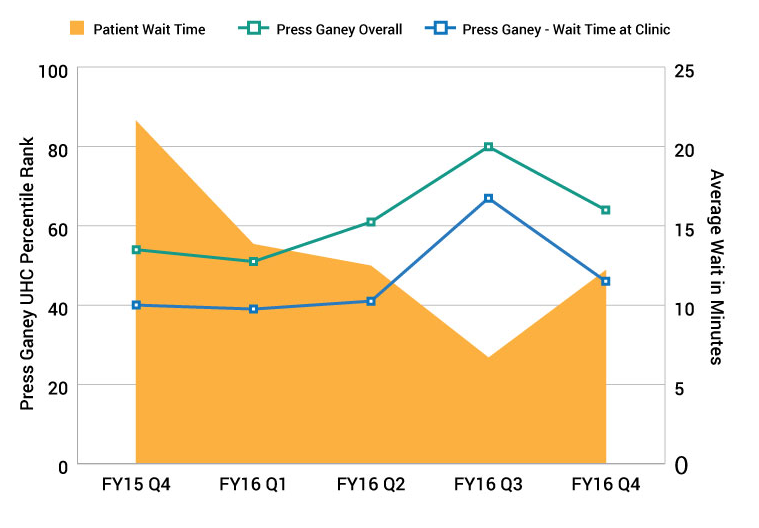
At the beginning of FY16, hospital leaders set a goal for Moran to increase their patient experience score by 15 percentile points (64th percentile to 79th). Moran’s leaders knew that they had to tackle their legendary wait times to make such a drastic improvement. Fixing wait time is the right thing to do and pressure from leadership accelerated change.
But where to start? Tinkering with patient volume was not possible—the Moran staff needed physician buy-in, and decreasing the number of patients meant decreasing physician compensation. Physicians would not go for that.
Moran's steps to understanding wait time
1. Start with the data
Patient Experience scores and comments indicated long waits, but it wasn’t clear what created the wait—did the techs take too long rooming patients? Were the doctors spending more time than expected with patients? Darden enlisted Casey Moore, the Eye Center’s quality improvement manager.
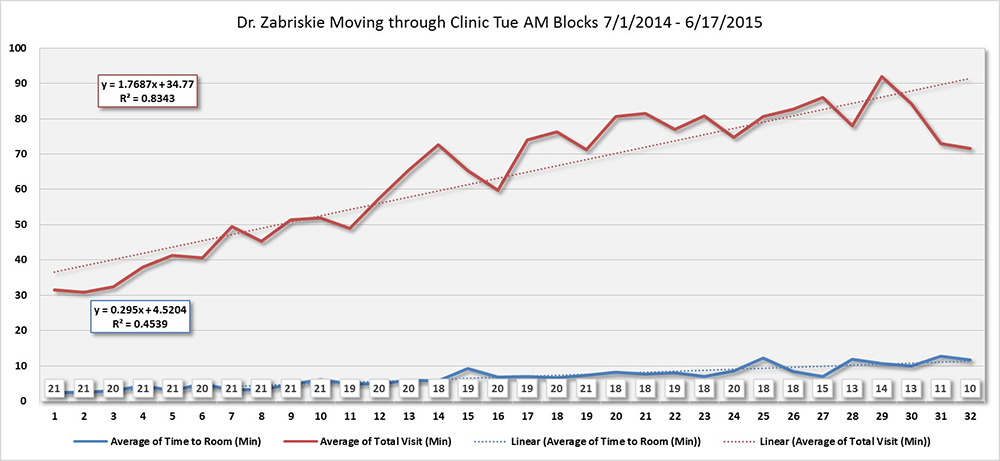
Moore began looking at the inputs of a visit. He discovered patients’ visit lengths increased as the day went on (below). Could the growing cycle time indicate a deeper problem?
What is "gemba?"
The gemba is a principle of Lean process improvement meaning “where the work happens.” The gemba are the physical locations where people perform the process. In this case, the gemba was the clinic rooms, hallways, and prep rooms.
Why go to the "gemba?"
The knowledge to improve usually doesn’t come from a conference room. This knowledge comes from watching the work before proposing solutions. Understanding the work is an important way to respect the people who do the work, followed closely by designing processes that allow them to succeed. Go see, ask why, and show respect.
2. Go to the "gemba"
Moore wanted to see the work in action. He observed several clinics held by Dr. Paul Bernstein, Dr. Judith Warner, Dr. David Dries and Dr. Robert Hoffmann. He needed to observe the clinic in action to see how, when and where delays were happening. Moore remembers “watching the clinic and talking with providers and staff helped me understand the flow in ways the data could not.”
3. Data and observation inform the soution
Moore, Darden and Marthia convened to discuss the data and observations. The team composition was important—Moore was a data analyst, Marthia had supervised providers’ clinics for years, and Darden would lead the transition with physicians. Marthia had worked on wait times in several previous improvement cycles and had been met by familiar responses from providers: “Of course patients are going to wait, they are seeing world-class doctors.” For years, providers blamed staff as a first line of defense. Marthia was relieved that Moore’s analysis showed that the tech staff were doing everything they could–completing intake quickly.
Marthia, Moore, and Darden discussed solutions. Many solutions could work, but could they be supported by Moran’s culture? One patient per appointment slot would not work. The team wanted template changes to feel unobtrusive—no added staff, no excessive late hours, no need for retraining staff, and no reduction in patient volume.
Close examination of the data revealed a potential solution that met these criteria—insert five minute pauses in the schedule at specific times. The idea was informed by queuing theory, the mathematical study of waiting in lines. The daily traffic jam in clinic is caused by minor variations in visit lengths. When the accumulated variations tended to reach a critical point, a short pause would give the clinic just enough time to clear the previous patients and avoid the oncoming jam. But if they only inserted one pause, they would have merely delayed the jam an hour. To avoid the jam completely, two more pauses would be required. Thus, all the appointments from 9:10 to 9:55 were pushed back 5 minutes, the appointments from 10:00 to 10:45 were pushed back 10 minutes, and the appointments from 10:50 through 12:00 were pushed back 15 minutes.
The team piloted their proposed solution at the retina clinic, where wait times were particularly acute for Dr. Bernstein, Dr. Michael Teske and Dr. Albert Vitale. They saw immediate results. Visit times increased more slowly throughout the day, and patients waited fewer minutes.
4. Crisp data analysis matters
With proven results, the team went to other providers. Most were very willing. Darden remembers that the providers were “wowed by the analysis.” Only one provider was hesitant. Darden offered to go back to the old schedule if there was a problem. After a few clinic days, the provider felt comfortable. “Giving an option to change back helped the providers feel in charge of their schedule, which is important for their engagement,” Darden comments.
"Every visit to the Moran eye center is a good experience with doctors and staff. Pleasant experience all around. Have been a patient for many years. There has been improvement in waiting time. Staff and doctors have always been stellar."—Visit June 15, 2016
"I have been in before with my mother and aunt several times and the wait time was always horrendous. I don't know how long I waited, but it was not long and very reasonable. Due to my previous experiences, I was expecting a long wait and brought a book. I barely had time to open the book."—Visit April 27, 2016
"I've never been to a place where everyone was so nice and helpful and seemed like they actually cared? You know, didn’t rush you through and paid attention to you. It threw me at first because after I was asked a question everyone waited for a complete response! I wasn’t sure how to handle it at first!"—Visit July 6, 2016
All patient comments were collected on Press Ganey outpatient services surveys, accessed for this article in September 2016.
Reflection
Ask any clinic manager, managing wait time is an ongoing battle. While the challenge is ongoing, Darden and the team took away a few lessons that translate into their improvement work, and their day to day operations:
- “If you want to see change, you have to change,” Darden states. “For years, we tried to address anything but the core issue of wait time. We made our waiting rooms better, we trained people how to talk about the wait, we offered snacks. We didn’t want to talk about changing a provider’s schedule. All of these changes were good, but they didn’t address the core issue.”
- As they worked through changing the templates, providers grew to trust that the team and the administration of the Center had shared goals.
- Lastly, the data analysis was crucial. Understanding the data and being able to speak to it was critical to communicating with the providers.
As waiting decreased, patient experience performance increased
Mari Ransco
Chrissy Daniels
Steve Johnson
Collette Marthia
John Darden
Casey Moore
Improving value in healthcare means redesigning care to meet patients’ needs. We must push ourselves beyond patient satisfaction surveys to reduce uncertainty, complexity, and confusion in the delivery of care. Matthew Stein, MD, and the Breast Imaging team unflinchingly faced a source of uncertainty for patients: waiting for mammogram results.
The following case study examines a new core competency in delivering value at a system level. At the University of Utah, leaders created integrated oncology teams organized for the patient. Collapsing historical silos and empowering front-line leaders grew adaptive teams that offered better value to cancer patients.
Why do some organizations thrive during a crisis while others flounder? Iona Thraen, director of patient safety, joined forces with her ARUP Laboratory colleagues to learn how the world-renowned national reference lab adapted to the pandemic. Leaders created a culture of safety by putting innovation, learning, and patient-centered care at the heart of all their efforts.