The Challenge
The Value Equation of Standardizing PCI Medications
Patients trust us to provide the right medication at the right time. By standardizing the drug cocktail given to PCI patients, University of Utah Health ensured that the right drugs go to the right patients, and that only the patients who need it receive a higher cost drug.
Utah’s value equation is defined by the patient, and it is Value = Quality + Service/Cost. This case study demonstrates improved quality (appropriateness of drug choice) and increased savings.
ealthcare is full of passionate people who choose their field because of motivation to help the sick and injured. That passion can lead to big, audacious goals, like ‘reduce obesity,’ or ‘improve vaccination rates.’ Starting small and growing slowly requires patience but can sway those with differing opinions.
Background
Dr. Theophilus Owan is an interventional cardiologist at University of Utah Health. Owan specializes in caring for patients with coronary blockages. He performs percutaneous coronary interventions (PCI), in which he feeds a catheter through the patient’s narrowed blood vessels to open them and increase blood flow. Bleeding is a perennial risk of this procedure.
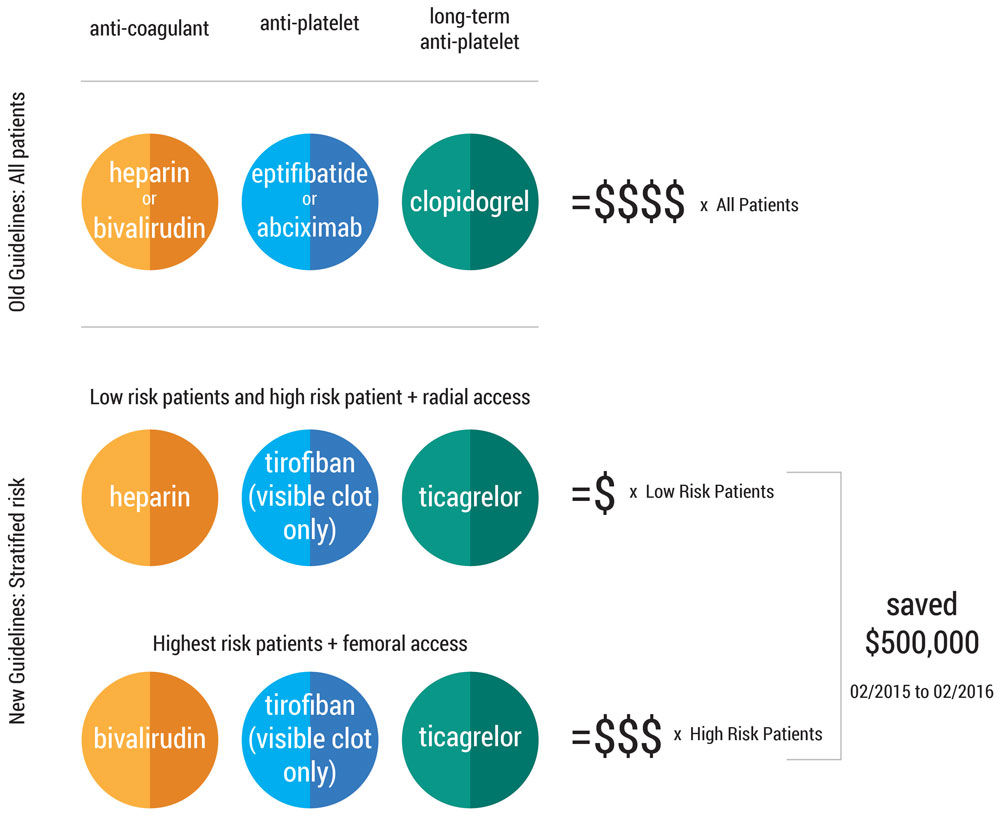
In 2014, Owan attended the American Conference of Cardiologists and watched a presentation that incited a fiery debate amongst his colleagues. A study from the United Kingdom compared two anti-clotting drugs used in PCI in a randomized trial. This study challenged long-standing practices that were actively supported by leading academic medical centers and pharmaceutical companies. Previously, physicians performing a PCI prescribed their choice of medicines to patients, regardless of bleeding risk. The new study indicated that different medications could be given to specific groups of patients with no change in outcome. By stratifying patients into a low-risk and high-risk bleeding groups, and then giving appropriate medications, drug costs could be reduced substantially.
Owan remembered, “It was radical! I really liked it. Up until 2014, there had been no head to head study. Now, these researchers were really challenging practice.” If Utah could create a similar drug protocol, the right patients would receive the right drugs with drastic cost reduction. Owan wanted to convince his colleagues to shift to a standard drug protocol.
"Supposed to be easy."
TOOLS TO CHANGE THE PRACTICE OF OTHERS:
#1: Gaining support from key individuals
#2: Don’t rely on the top-down hierarchy. Meet with colleagues and discuss.
For another case on changing the practice of others, read "How a Hospitalist Duo and a 1000-person Multidisciplinary Team Changed Practice."
Owan and his section chief, Dr. Fred Welt, decided to bring the study to the cardiology group. Welt wanted to standardize Utah’s practice for all PCI patients, approximately 300 patients per year. Cardiovascular division chief, Dr. James Fang, also advocated for a “Utah way” of reducing unnecessary variation in practice. Owan signed up for the Value Improvement Leaders course for guidance. Value Engineer Cindy Spangler began coaching Owan with value improvement principles.
“Cindy has been instrumental,” Owan commented, “Cindy has helped me focus. She helped me see the process of change.”
Owan and Spangler identified the other stakeholders in a PCI patient’s value stream (the emergency department, pharmacy, cardio-thoracic surgery) and chose to start with his own group: interventional cardiology. Just like at the national conference, heated debate ensued. “With real naiveté, I brought the article to the group. It was supposed to be easy,” Owan remembered. “There was literature...but if you put two or three cardiologists in a room, well, there was opposition. It was very strong.”
“There was literature...but if you put two or three cardiologists in a room, well, there was opposition. It was very strong.”
Some cardiologists hypothesized that the savings would evaporate if patients ended up staying longer in the hospital should surgery become necessary. Physicians in the emergency department, the entry point of PCI patients, were also skeptical. ED physicians expressed that cardiology changed protocols frequently, and this change was just one more in a long line. There was no consistency, they complained. Why change again?
Owan discovered that sharing the article with his colleagues was not enough to change minds. The physicians had read the same literature, yet had come to different conclusions about practice. Owan recognized the need to discuss their interpretations. He commented “The literature and the data won’t change minds. People have different conclusions from literature and it takes convincing. Sometimes you have to bring out specific parts to make your case. Don’t assume that people know the literature or understand the literature the way you think they do.”
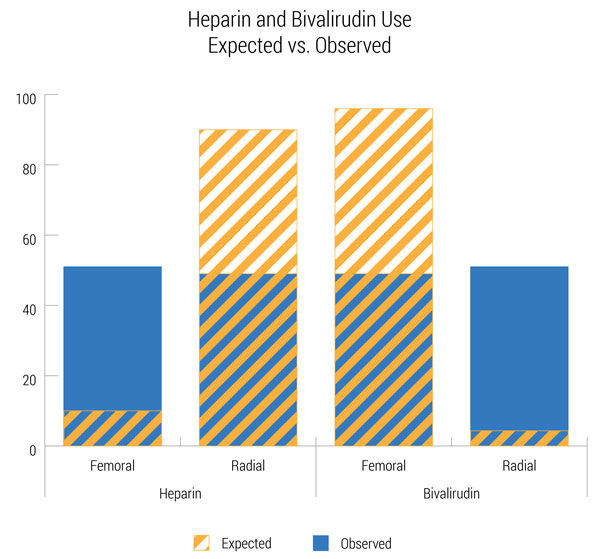
Owan began to meet individually with the cardiologists to discuss the new idea–a standardized drug protocol stratified by bleeding risk. He met with his most vociferous opponent to the protocol first, and brought Utah’s own data to demonstrate the need for change. The data surprisingly revealed wide variation in practice. Practice guidelines were frequently discussed, and yet physicians’ individual choices did not always follow the guidelines. Owan commented “Everyone knew the practice guidelines. Our education of fellows is based on guidelines. But then you see it doesn’t happen that way. Its totally opposite. We were very random.”
Baseline analysis indicated prescription variation
New guidelines: Stratified risk
The Power of Scope
Improvement principle used: Scope
Projects can be scoped and bounded in several ways:
• Physical Areas
• Geographically
• Work Scopes
• Organizationally
• Data
• Product
• Customer
• Time/Level of Effort
Owan and Spangler proposed limiting the scope of the drug protocol to STEMI patients, a sub-group of PCI patients who are experiencing an especially serious heart attack. With their own data, the literature, and the limited scope, Owan convinced the key opponent that the protocol was worth a try. The unified front convinced the larger physician group. They approved the first trial of the new protocol (see sidebar “Scoping is important, but let’s not forget implementation” for the rest of the implementation story).
In the process improvement world, we call this scoping your project. We have a partiality for big, splashy changes to fix a problem immediately. But, splash can be antithetical to the long-term practice change needed to sustain value improvement. Owan scaled back his initial scope by 90% (from 300 PCI patients to 30 STEMI patients).
As he talked about the protocol for STEMI patients, he also made sure to include how the new protocol could work for more patients. Owan remembered “I made sure I was circulating the literature to make people realize it would be effective beyond the STEMI population. Just do STEMI first.” Owan had his sights set on the long term vision – a standard protocol for all patients undergoing PCI. After the first year of data showed the protocol was effective, he and Spangler expanded the scope to include NSTEMI patients, then all PCI patients.
Systematically expanding the scope
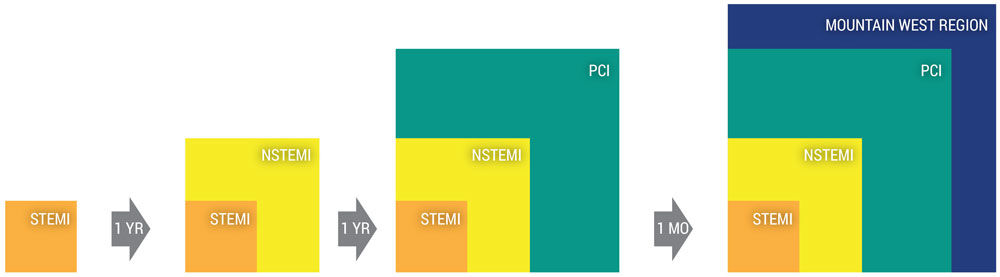
Most recently, Owan has worked to change practice in the surrounding Mountain West region. Patients needing a PCI often come by AirMed to the main University Hospital. Owan is working to reconcile the new protocol with our partner hospitals through incremental but important steps. For example, patients would often receive a convenient, yet problematic, shot of enoxiparin en route to Utah’s hospital. Once at Utah, it was a “nightmare to get everything right. If a patient had received the shot, the rest of the care was very finicky,” remembered Owan. Owan began to ask referring facilities to give heparin in IV form, and helped them work through process issues such as pump and bag usage. “It has been amazing, we are able to help people much more quickly,” Owan said.
Owan is also working with some affiliate regional hospitals to adopt the new drug protocol. Memorial Hospital of Sweetwater County in Rock Springs, Wyoming is the first affiliate to use the new protocol in an effort to provide continuity of care if the patient needs to be transferred to Utah. This type of geographic expansion is a great example of spreading value for patients throughout a given region.
Reflection
After one year of implementing the new protocol for all PCI patients, cardiology has saved nearly $500,000 in drug costs and improved the appropriateness of medications. This change has not been easy. Changing the practice of peers is challenging. It requires a willingness to discuss different interpretations of evidence and a commitment to experiment.
Dr. Owan implemented a new protocol in a small and specific population, convincing his peers meant expanding slowly. Like in many improvement cycles, success has come in successive rounds.
Scoping is important, but let's not foget implementation
While convincing the doctors to agree on the standardized protocol was a hurdle, implementing a seamless process required a wider team.
Pharmacist Teshia Sorensen led the pilot’s implementation across the hospital’s inpatient units, cardiac catheterization lab and emergency departments at the main hospital and South Jordan campus. She prepared the new protocol for submission to the pharmacy and therapeutics committee. She and Dr. Owan presented the protocol to the committee and obtained approval to implement. The protocol standardized treatment regimens for patients before they arrived at the cardiac catheterization lab (i.e., in the emergency department), during the PCI procedure, and after the cardiac catheterization (i.e., on the inpatient unit and after hospital discharge).
Because the new protocol required drugs that the hospital did not use regularly, several steps needed to occur prior to implementation to ensure the protocol would succeed. Sorensen worked with pharmacy buyers and drug distributors to obtain sufficient amounts of each drug to support the anticipated patient volume. She worked with inpatient pharmacy to update each unit-based drug repository (Omnicell) to ensure that the correct drugs were on hand in appropriate amounts. She created STEMI kits with the pre-cath lab drugs so that emergency room staff could grab them quickly as a STEMI patient arrived. She worked with IT pharmacists to program the right doses and directions into the Alaris smart IV pump library and into Epic orders and order sets to ensure each drug would be ordered and administered appropriately.
Finally, Sorensen educated physicians, nurses, and pharmacists throughout the main hospital and the South Jordan emergency department on the new protocol prior to implementation. She also met with nurse educators to ensure ongoing education would reflect the new protocol.
Sorensen repeated her effort as they moved from the STEMI cycle, to the NSTEMI and then full PCI cycles of implementation.
Read the official guidelines here
For referring hospitals:
STEMI or New Left Bundle Branch Block Transfer Protocol
nstemi or unstable angina transfer protocolNSTEMI or Unstable Angina Transfer Protocol
Accessible for University of Utah Health only:
Mari Ransco
Chrissy Daniels
Cindy Spangler
Steve Johnson
Teshia Sorensen
Theophilus Owan
Chief Quality Officer Sandi Gulbransen and Accreditation Manager Kemper Funk explain how this umbrella of standards—ISO-9001—relates to our accreditation process and impacts our daily work.
SMART Goals are a great starting point for any project. Project management expert Kripa Kuncheria helps us organize our teams’ efforts by outlining this goal setting framework with a simple step-by-step guide to try right now.
Pediatric hospitalists and patient advocates Reena Tam and Erin Avondet shed light on the untapped opportunity to augment pediatric vaccination coverage in our communities and build vaccine confidence in the inpatient setting. They provide a host of resources and practical tips you can apply right now.