What is a Bundled Payment? (Quick refresher)
In a prior Accelerate post, we defined “bundle” as the placement of all the care for a certain procedure or series of procedures into a single bucket. The rationale for contracting for a bundle is threefold:
- Patients benefit from having a team of providers focused on improving care processes, which often result in reduced procedures, supplies, and transition time.
- Payers benefit from having a pre-determined price they will pay for care, meaning they know the exact amount they will pay for an episode of care.
- Care providers benefit from knowing the predictable amount they will get paid for patient care, even if the costs associated with that care are under the agreed-upon set bundle amount.
BPCI Advanced
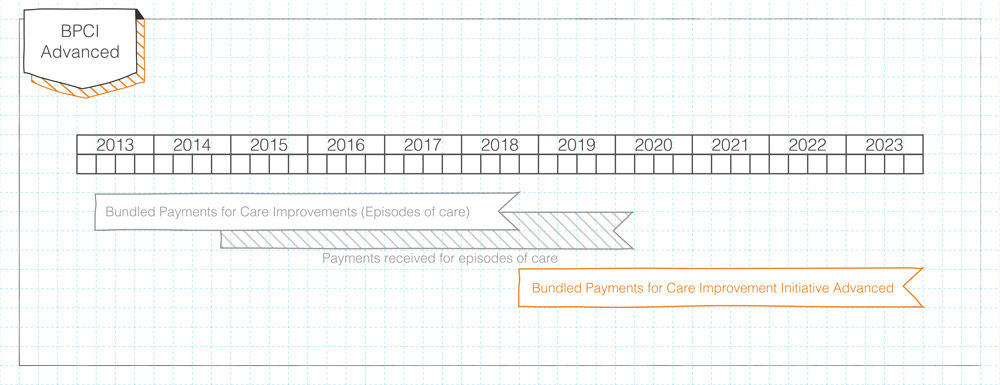
On January 9th, 2018, the Centers for Medicare & Medicaid Services (CMS) announced a new bundled payment program: the Bundled Payments for Care Improvement Advanced (BPCI Advanced)CMS continues its lack of originality when it comes to naming programs. Come on, BPCI "Advanced"? Why not just go with "Super BPCI" or "BPCI Platinum Edition"?. The program officially begins on October 1st, 2018 and continues until December 31st, 2023.
Background
CMS’ original BPCI program began in 2013 and is slated to end in September 2018. The announcement of this new program to take the “bundled baton” has been anticipated for months, meaning BPCI Advanced did not catch anyone by surprise. CMS is still releasing details of the program, but since the application deadline is March 12th, interested organizations need to act quickly with the knowledge at hand..
How is “Advanced” different?
For the sake of brevity I’ll highlight the main differences between the original BPCI program and this new advanced one. The list below illustrates these differences, though I want to highlight a major one: the fact that CMS “expects” (their word) this program to qualify as an Advanced Alternative Payment Model under CMS’ Quality Payment Program (QPP).
QPP is a complex program, though at a high level, CMS will potentiallyDepending on how a system performs across the Merit Incentive Payment System (MIPS), the track within QPP that runs parallel to APMs, a system could potentially be paid more than if they are part of the APM track. There's a very slim possibility of that happening, though. reimburse providers and systems more based on whether or not they are involved in one of CMS’ “Advanced Alternative Payment Models” listed in Table 1. As a system, we have elected not to participate in any of these models, so the BPCI Advanced program presents us with another option for participation, albeit a slim oneFor a group of providers to qualify as an Advanced Alternative Payment Model, a certain percentage of patients or dollars billed under the Tax Identification Number need to be above 20-25% in year 1 of the program. These numbers climb to 50%+ by 2022..
CMS’ Advanced alternative payment models (updated in 2017)
- Comprehensive ESRD Care (CEC)—Two-Sided Risk
- Comprehensive Primary Care Plus (CPC+)
- Next Generation ACO Model
- Shared Savings Program—Track 2
- Shared Savings Program—Track 3
- Oncology Care Model (OCM)—Two-Sided Risk
- Comprehensive Care for Joint Replacement (CJR) Payment Model (Track 1- CEHRT)
Unraveling Payment
A whole lot more on bundles:
A Post About Nothing (sort of)
Differences (Compared to original BPCI program)
- There are inpatient (29) and outpatient episodes (3)—BPCI only consisted of inpatient
- Quality measures have been added to the program that will affect potential incentive payments (+/-10%)
- Post-acute providers are not allowed to be “initiators” in this program
- The “discount” CMS takes when calculating potential savings has been increased to 3% (from 2%)
- Learning activities will be “mandatory,” meaning CMS is trying to make health care providers collaborate in formal ways to share cost-reduction processes
- Only two payments per year (compared to four)
- A single risk track, slated to be the 1st/99th percentiles (compared to three risk tracks)
What to do
While details are still emerging—the exact benchmarking method, for example—health systems and physician group practices should apply for the program to gain access to their own historical data. That information alone is quite valuable, even if the applicant ultimately decides not to participate.
Potential applicants should:
- Assess their internal trends for volumes, costs, and quality measure performances across the applicable DRG/HCPCS codes
- Assess their historical data from CMS across the same metrics
Based on the findings from the points listed above, potential participants can decide which episodes to select for participation—or simply not participate at all.
Three last points
- A group has until August to formally commit to the first phase of the program (starting October 1st, 2018)
- If a group decides to not start the program in phase I, they can join the program in January 2020
- This is a voluntary program, meaning a physician practice group or health system can leave the program at any point
Zac Watne
Intensive Outpatient Clinic Physician Stacey Bank, Social Worker Christina Cackler, and Executive Medical Director of Population Health Peter Weir share what it took to build an integrated practice and why it pays to innovate for patient-centered care.
It’s a truism: the cost of care is unsustainable. But what’s the fix? In this new series for Accelerate, Zac Watne, Senior Manager of Payment Innovation, interviewed U of U Health leaders to get their thoughts on one of the most controversial fixes making headlines: Medicare for All.
Patients will ask three things of us over the next decade of health care improvement: help me live my best life, make being a patient easier, and make care affordable. To meet those needs health care must shift—from organizing around a patient’s biology to understanding the patient’s biography.
