wasn’t until I became a practicing nurse that I realized how important the team is. When I started nursing school, just barely out of secondary school in India, I was surprised at how hard it was to care for people. Patients are experiencing one of the most challenging times in their life, and it is often messy and hard. Gradually, I realized I could study and get good grades on my own but taking care of another human being requires a team. Nothing can be done alone. Excellent care includes the patient, nurses, and other care providers all working together.
Leading a team has its own challenges and learning to work effectively together is a never-ending process. I love to learn and try new things, but they always rest on two principles—being clear about my intent and supporting my team.
1. Be clear about your intent
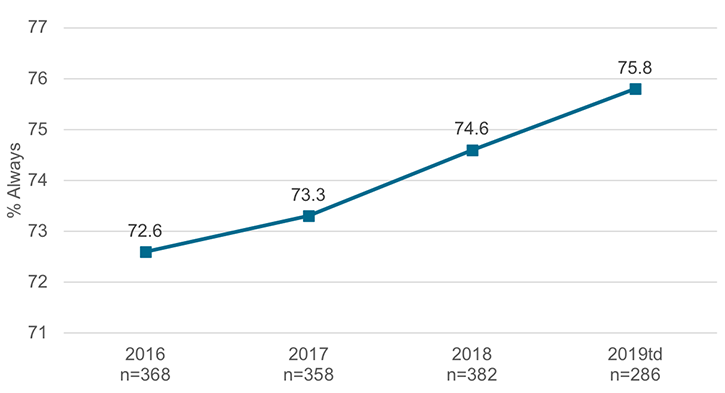
Our intent is not achievement of metrics. Our intent is to strive for excellence. When I first opened the Internal Medicine unit (West Pavilion 5, now known as Internal Medicine A50) four years ago, I was coached to think carefully about how I wanted my patients to feel, and then let that vision guide the team and environment.
My core value was and is safety. I want our patients and our teams to be safe and importantly, feel that they are safe. Being clear about my vision helped me be clear with everything else. It has informed how I’ve hired the team, and how we talk about what is important to us. Safety means treating everyone as a person, not as a room number. I expect everyone to deliver honest and compassionate care.
There is no cookie-cutter for what a patient wants. As a manager I set the bar high and expect excellence from everyone on my team. I work to be transparent so people know what to expect and trust that I will do what I say. If you’re true to what you feel, you can deliver what your patients want. Patients want and need a good human around them. We have to constantly re-evaluate our processes to support that and be ready to try new things.
Two ways to make it easier:
Daily Rounding: “How are you today?”
One of the most important things I can do as a leader is know and love my people. With nearly 100 staff on my team it might seem impossible to get to know each of them individually, but it’s not as hard as you might think. I implemented a system of “daily rounding” with staff (and sometimes patients as well) to interact with every team member.
I spend the first two hours of every day on these rounds. There are no set questions, just a simple “how are you doing today?” I want to listen to their verbal cues and watch for their nonverbal cues in the response. Sometimes I walk into a patient room to refill their water or help them to the bathroom. It’s not about checking a box that says I visited with this many people this many times, it’s about connecting, being present, showing my staff that I am here for them and I truly care.
Empowering the team
Once we’re clear about our shared intent and we have regular channels of communication, we can work to improve together. I’ve empowered our nurse practice council to identify the challenges that are most important to them, and then we solve together. The council includes everyone on the unit, RNs and HCAs. There is a new leader of the council every two years, and right now it's McKay. It’s a path to leadership on the unit.
Every year, we talk about what we want to work on and every year, we reflect on what we’ve achieved.
2. Support your team—be interested, be available
One of the biggest challenges we see is nursing turnover. Today, about 90% of my staff are members of the millennial generation. Rather than feeling frustrated with workplace behaviors I didn’t fully understand, I decided to find out everything I could about their motivations and habits so I could meet their needs and they could focus on meeting patients’ needs. Coupled with mentally and physically challenging work, our turnover rate was as high as 50%. It makes it hard to have consistency in patient care, and we saw that in our patient feedback.
What I learned is that millennial workers value their time away from work, they use technology seamlessly in their everyday lives, and they like immediate feedback. I took that information and made changes to the operational flow of our department.
Two ways to make it easier:
Share the “why” behind the work, frequently
We implemented a new hire training every six months that I always attend. I want to get to know my new nurses and help them get to know me as a person, not just someone who cares about numbers and scores. We talk about your why—why are you here? I tell them to be completely honest. They don’t have to say it’s because they want to care for patients; it could be the tuition discount, or earning money to buy a new car. We don’t make people share their why publicly and there’s no judgment of anyone’s why. I’ve found that when we let people be true to themselves, they will be true to our patients.
We spend the remainder of the training exploring the reasons behind the things we do and tools for success. These trainings have reduced our turnover rates and increased the quality of our care.
Adjust meetings for convenience and meaning
I reduced the number of required meetings from monthly to quarterly, so staff only have to make time for four meetings a year. We’ve turned those meetings into mini-retreats so that it's not just information sharing, we’re actually discussing issues together.
With only quarterly meetings, it’s critically important that everyone attends each one. We put the retreats on people’s calendars at least three months in advance. We schedule a morning and evening session so everyone can attend and it won’t interrupt patient care. They’re scheduled in the education building, so they are a true retreat, with food and fun, in a safe environment.
Each retreat is centered around three questions:
-
What do you need? The team identifies things that they want to work on or are struggling with, and these become our focus.
-
How are things going? We talk openly and monitor progress since the last quarterly retreat.
-
What are we celebrating? I show them how much I appreciate the success we have achieved together. They work hard and deserve to know that we see it.
We also changed the way we communicate to better fit our workforce. Since most of the staff prefer electronic communications, we text and send out e-newsletters, which has increased engagement and understanding.
The hard work is worth it
I know that we can’t please every patient every time, and I know that part of being in nursing means accepting that some of our staff are going to leave. Do I feel sad when I invest the time in a new staff member who decides to leave? Absolutely. But if we can plant a seed that helps every nurse be a little better, that makes our whole organization better in the end. By acknowledging these realities, I can make better leadership decisions for my team, and therefore for patients.
Internal Medicine A50 RN Communication
Shegi Thomas
Hospitalist Ryan Murphy reflects on the care his dad received as one of Utah’s first hospitalized COVID-19 patients. The experience shaped how he communicates with patients—whether or not they have COVID—in spite of isolation, masks, and physical distancing.
Learning to listen is not only a leadership skill—it’s a life skill. Leadership training specialist Jess Burgett shares three practical tips for harnessing the power of listening with intent.
Its that time of the year, when respiratory illnesses are common. Masking is one way we can protect our most vulnerable patients and ourselves. Use the below guide to discuss masking with your teams and with our patients.